Strategic demand and capacity model incorporating patient flow for adult mental health crisis pathway
Surrey and Borders Partnership NHS Foundation Trust and Surrey Heartlands ICS needed a clear, strategic view of how future demand and resources required to meet future population MH needs would evolve across their adult mental health crisis pathway. Pressures on inpatient beds, increasing out-of-area placements, and limited insight into future workforce and capacity needs made long-term planning difficult. CF were commissioned to developed a dynamic modelling tool which incorporated patient system wide flow to help the Trust understand and plan for future capacity and workforce requirements — now used to support scenario testing and business case development.
What was the challenge?
Surrey and Borders Partnership NHS Foundation Trust (SaBP), working in collaboration with Surrey Heartlands ICS, sought to strengthen long-term planning across the adult mental health urgent and emergency care (UEC) pathway. Like many systems nationally, they were operating within a context of growing and increasingly complex demand, fixed inpatient capacity, and increasing reliance on out-of-area placements. Community crisis services were playing a greater role in responding to need, and there was a clear desire to understand how different parts of the pathway interacted and responded to crisis.
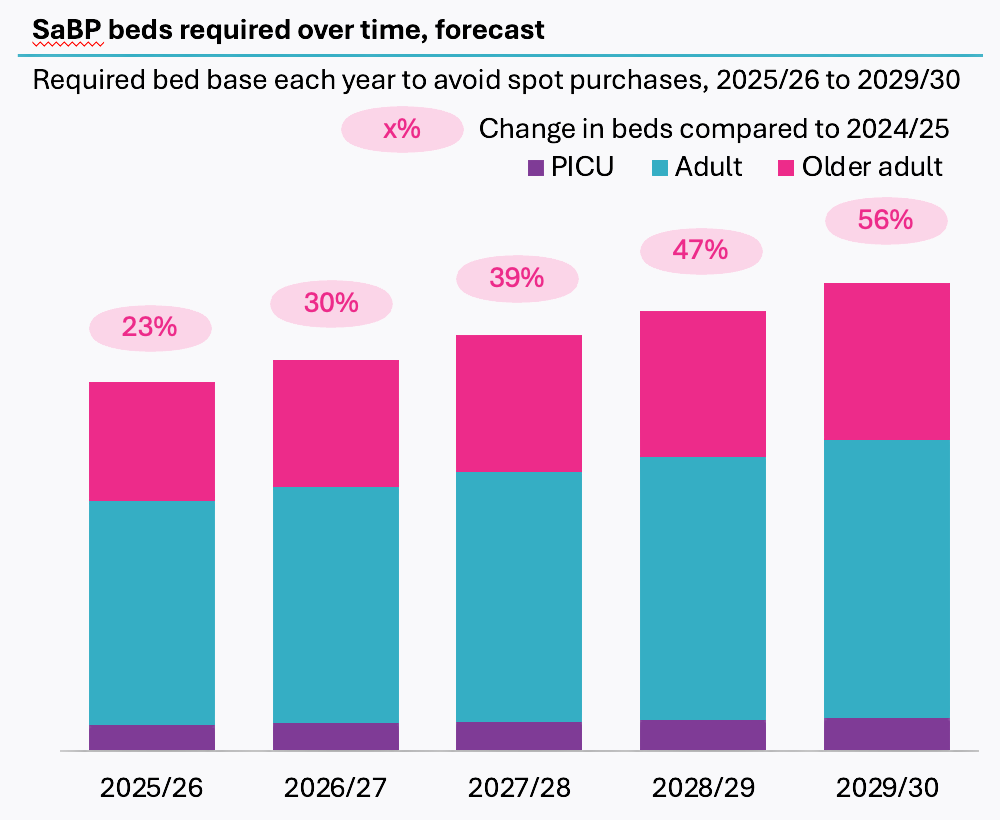
While a wide range of data existed across services, there was no single, integrated tool to forecast future system needs or to test how potential ‘flow’ changes — such as increase community services, adjusting bed base, reducing length of stay, or increasing productivity — might affect capacity and resourcing. To support investment planning and strategic decision-making, the Trust required a forward-looking, evidence-based model that could be adapted over time and used internally by analytics and planning teams.
What did we do?
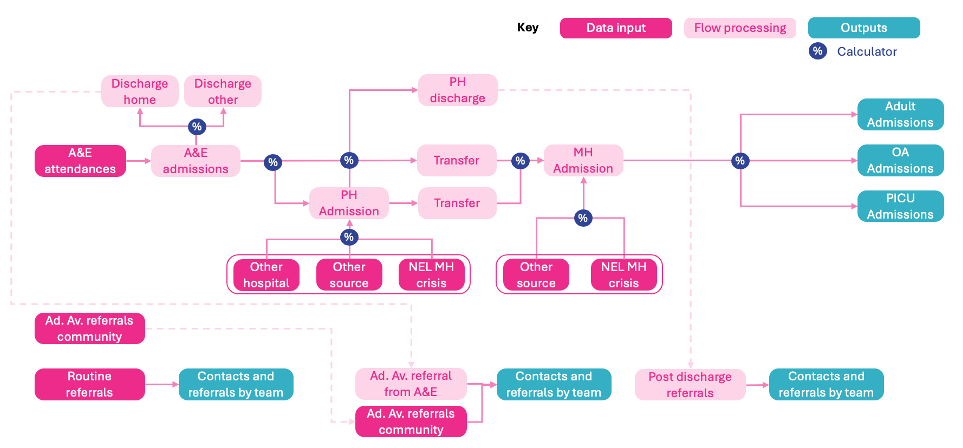
We created a dynamic model to help SaBP and the ICS plan across its adult mental health urgent and emergency care pathway. Based on the existing patient flow, the model connects activity data from A&E, inpatient services, and community teams (pre and post admission). This gave a clear picture of how patients move through the system and how changes in one area — like an increase in community capacity — might affect others.
To ensure the model could be used effectively by internal teams, we focused on accessibility and transparency. Users can easily change key assumptions, such as average length of stay or the number of daily community contacts, and instantly see how those adjustments affect workforce needs and physical capacity. Inputs, variables, and outputs are separated cleanly within the tool, making it simple to navigate, test scenarios, and generate meaningful insights.
In addition to the technical build, we delivered supporting documentation, training and a built-in SQL refresh process to enable the the model updated on a frequent basis with new data. The result is a flexible and sustainable tool that supports strategic planning through the running of scenarios supporting the development of business cases over time — all within the analytical environment that the organisation can update.
What was the impact?
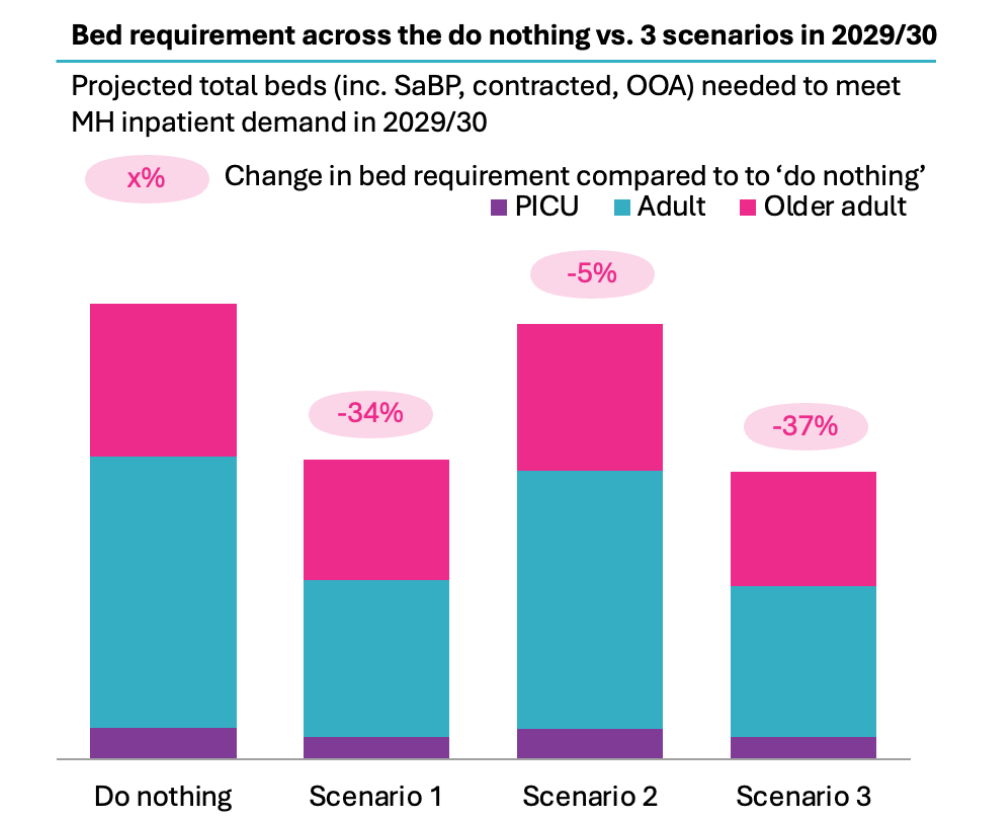
The greatest impact of the model was the ability to run scenarios for new care models or flow. Using targets identified through best practice, historic achievement and national guidance, the model user can adjust both operational and efficiency parameters of the model under a ‘do something’ scenario. This shows how under a scenario where that target is achieved, what the requirement in terms of beds and workforce would be required. The scenario can then be compared to the ‘do nothing’ scenario to understand the benefit of achieving the target and associated financial savings. Running the ‘do something’ scenario multiple times under different parameters to create various scenarios allows the model user to compare and contrast the impact of different interventions side by side.
As part of the project we applied 3 scenarios, in addition to the baseline ‘do nothing’ scenario.
- Scenario 1 focused on reducing mental health inpatient length of stay (LOS) using 2019/20 values as a baseline with 2023/24 demographics, testing LOS reductions of 30% for Adult wards, 4% for Older Adult wards, and 21% for PICU wards.
- Scenario 2 examined reducing A&E attendances by 19% through expanded community crisis capacity to understand the impact of redirecting mental health demand from A&E to community services.
- Scenario 3 combined both interventions simultaneously to test whether the benefits could be realized together and identify any synergistic effects.
CF delivered a dynamic demand and capacity modelling tool that has transformed our approach to strategic planning for mental health crisis services. Thanks to this tool, we can now make strategic decisions such as investment in inpatient and community services using a data-driven and comprehensive approach that considers the end-to-end patient flow on the pathway. The CF team also supported us throughout the development and handover of the tool to make sure we have the internal capability to use the tools and insights going forward. Overall, CF team have been very passionate about making this work a success, supported us closely every step of the way and brought a range of key stakeholders along on this journey with us.




