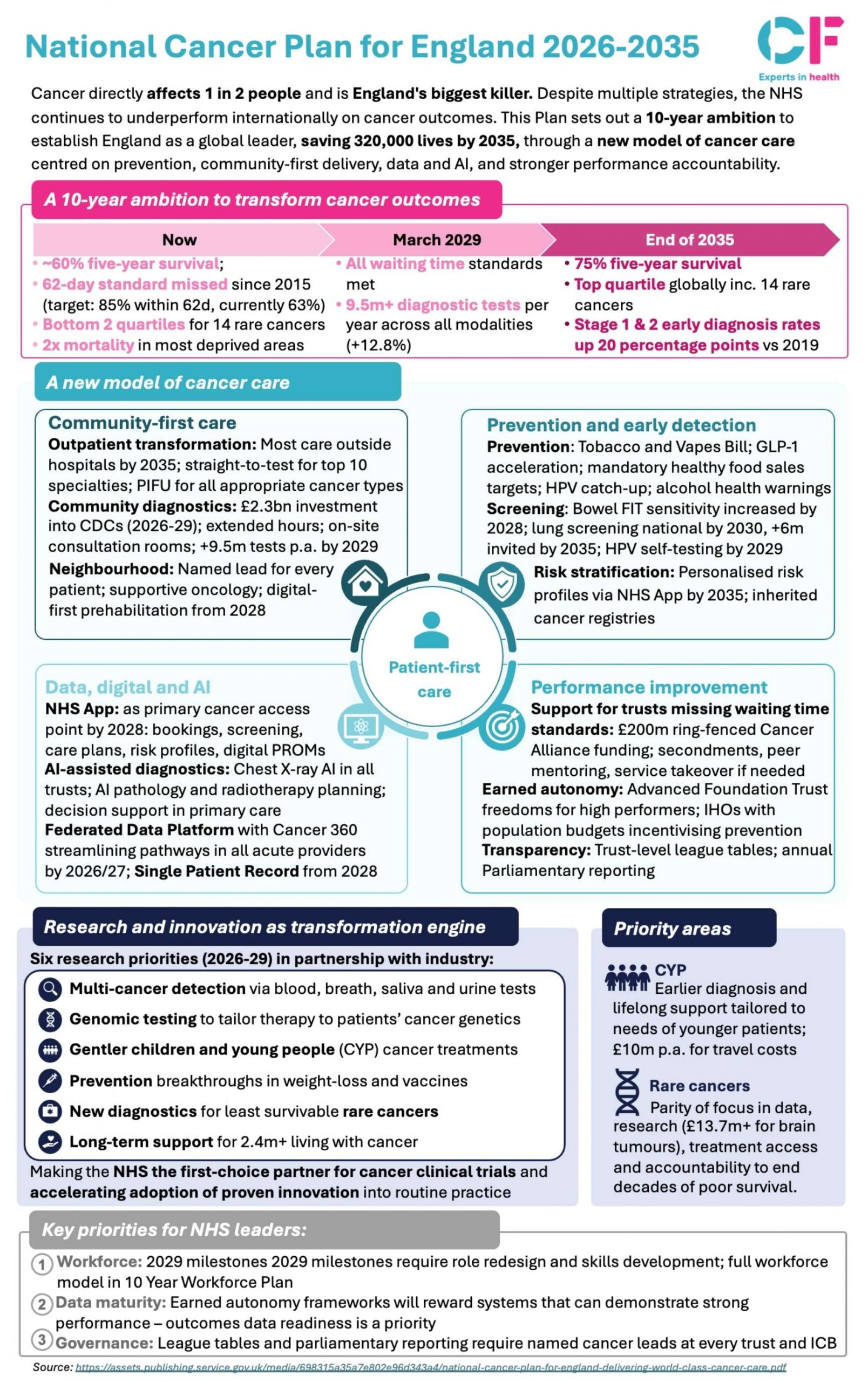
Cancer remains England’s biggest killer, affecting 1 in 2 people during their lifetime. Despite years of investment and strategy, the NHS continues to underperform internationally on cancer outcomes. The newly published National Cancer Plan for England 2026-2035 represents a significant shift in approach, setting out an ambitious 10-year mission to establish England as a global leader in cancer care by 2035, with a target of saving 320,000 lives.
This plan acknowledges past shortcomings head-on. Since 2015, the NHS has missed the 62-day cancer treatment standard, and outcomes for 14 rare cancers remain in the bottom two quartiles internationally. The plan seeks to address these challenges through a fundamentally new model of cancer care.
Key points from the plan
What it means for the NHS
This plan represents a fundamental restructuring of cancer services. NHS leaders face three key priorities: developing workforce capacity, achieving data maturity, and strengthening governance structures.
The shift to community-first care requires significant investment in diagnostic infrastructure and workforce redistribution. Challenged trusts will face unprecedented intervention, including secondments, peer mentoring and potential service takeovers. High-performing organisations will gain earned autonomy and AFT freedoms, while ICSs with population budgets can incentivise prevention.
The plan demands transparency through trust-level league tables and annual Parliamentary reporting. Cancer Alliances receive ring-fenced funding, but with clear performance expectations attached.
What it means for patients
For patients, the plan promises faster access, better outcomes, and more convenient care closer to home. The 9.5m annual diagnostic tests by 2029 should reduce waiting times significantly, while digital-first pathways mean booking, screening, and care planning through the NHS App from 2028.
Early detection initiatives, particularly multi-cancer blood tests and expanded screening, offer the possibility of catching cancers before symptoms appear. Named lead contacts and neighbourhood-level care should improve the patient experience and reduce the burden of travel to distant hospitals.
For rare cancer patients and younger people with cancer, the explicit focus on closing outcome gaps represents long-overdue attention to historically underserved groups. The emphasis on personalised treatments based on genetics points toward more targeted, potentially less gruelling therapies.
The success of this ambitious plan ultimately depends on execution. With 320,000 lives in the balance over the next decade, the NHS faces perhaps its most important healthcare transformation challenge to date.
See the full snapshot below: