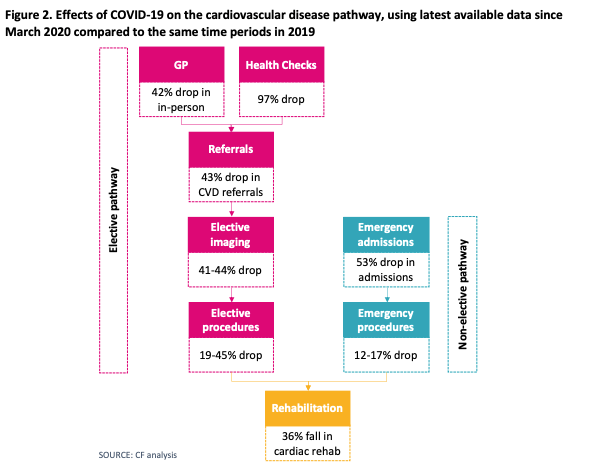
The burden of cardiovascular diseases (CVD) is huge in the UK. Approximately 7.6 million people in the UK are affected by CVD, which accounts for approximately 164,000 deaths per year. COVID-19 has substantially impacted CVD management across the board, including prevention, referrals, diagnosis, treatment and rehabilitation. In particular, health checks have dropped by 97%, which is a significant indicator of a decrease in screening and prevention, and consequently, to the initiation of preventative medicines, especially statins. While the shift to virtual appointments has been celebrated, in-person primary care attendance has decreased by 42%, which has significant implications on procedures that traditionally need in-person presence, such as measuring blood pressure and performing pulse checks. CVD referrals have also dropped by 43% which means that patients are not being referred for further specialist opinion. Indeed, this disruption has affected CVD services across the pathway, with a 19% to 45% reduction in elective procedures, a 41% to 44% drop in elective imaging, a 53% decrease in emergency admissions, and 36% drop in cardiac rehabilitation group exercise.
The headline figures from this mean
- Due to the missed activity, up to 470,000 patients will not have been started on statins, anticoagulants, other cardiovascular drugs or diabetes drugs
- As a result, 12,000 future heart attacks or strokes that could have been preventable might occur
- Additionally, the delays in diagnosis could result in 23,000 missed heart failure diagnoses, between 16,000 and 57,000 missed atrial fibrillation diagnoses, and around 26,000 to 90,000 missed coronary heart disease diagnoses.
What needs to be done to address this now?
- The obvious answer is the recovery of services, which will be a major undertaking. This would entail recovering GP services, elective services, and diagnostic capacity – especially echocardiograms – as well as strengthening stroke and cardiac rehabilitation.
- This recovery needs to be run in parallel with the embracing of innovation to its full potential. This should include a move to more effective digital solutions beyond telephone and greater provision of real-time data that can lead to improved responses to emerging healthcare challenges.