It is now well understood that Covid-19 has not just extracted a terrible toll on the elderly population but that it has also had a disproportionate impact on minority groups. In this report, we examine what the impact has been and also what we can do about it.
Black and Asian communities have been disproportionately affected by Covid where death rates are 3.3 times and 2.4 times higher respectively among black men and women than among their white peers. If the white population had the same risk of death from Covid as that faced by the black population at least 58,000 more people in England and Wales would have died to date from the virus.
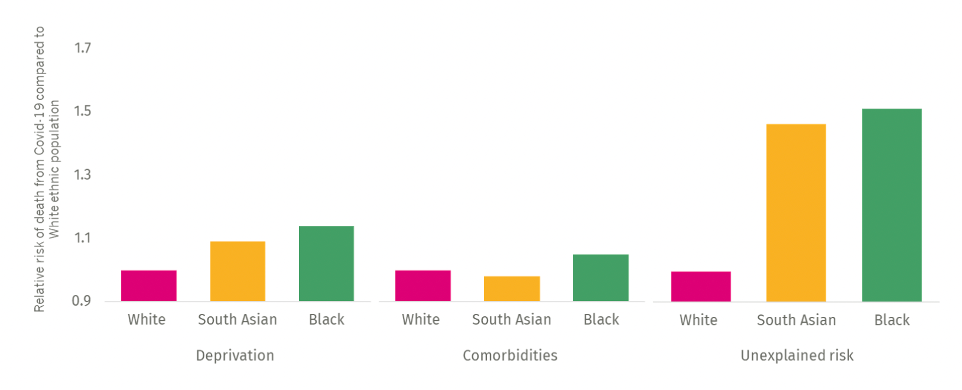
Our analysis shows that co-morbidities and deprivation account for only a small proportion of this difference. There must be other unobserved confounding factors at play. To try to understand why, we have made use of the new ECDS dataset to analyse the emergency care and critical care pathway for patients with Covid diagnosis, although in 89% of cases the coding of ethnicity is not complete.
What the analysis shows is Black patients in particular as well as South Asian patients are more likely to be admitted to hospital, be admitted to ICU, and be mechanically ventilated – each of which implies presenting to hospital with more serious conditions and these more serious conditions requiring greater escalation. Additionally, we find that Black patients have a 7.6% increased fatality rate in critical care.
Many have written about this on both sides of the Atlantic and suggested that key reasons for this excess risk is that Black patients, and to lesser extent South Asian, are presenting later for care and also then getting worse care.
- Patients may present late for a host of documented contextual reasons including lower health literacy, cultural reasons, greater difficulty in accessing care, challenge of building a therapeutic relationship with predominantly white professionals and a hesitancy to present due to a lack of trust.
- The care they then receive may suffer from a number of documented factors including unconscious bias of staff in the care they provide and care pathways not being tailored to the specific physiological and cultural needs of Black and Asian patients.
- We also recognise that underdiagnosis of co-morbidities in Black and Asian communities along with potentially increased physiological risk may be contributing factors.
To address these issues we recommend five actions:
- Routine collection of ethnicity data and equity of access to drive change.
- Incorporate a lens on ethnicity in all targets and performance.
- Work with Black and Asian communities to co-design clinical services and interventions.
- Concerted action to better protect ethnic minorities from the impact of deprivation on Covid risk.
- The NHS and LA as local anchor organisations need to work together to coordinate local services, ensure they meet the needs of their populations and positively impact the social determinants of health.