The NHS stands at a critical juncture. With public satisfaction at just 21% – down from 70% in 2010, mounting pressures from an ageing population and tough financial constraints, the need for fundamental reform has never been more urgent.
In response, the government’s NHS 10-year Plan aims to reinvent the health service while maintaining its core principle: free at the point of use. Born from over 220,000 public and staff contributions, the plan leverages the digital health revolution, genomics and AI to deliver three transformational shifts: from hospital to community, from analogue to digital and from treatment to prevention.
Key headlines
Three major shifts:
- From hospital to community: More care closer to home, with Neighbourhood Health Services and co-located centres open 12 hours a day, 6 days a week. Two-thirds of outpatient appointments (currently costing £14bn) will shift to digital alternatives, while 95% of complex patients will have universal care plans by 2027.
- From analogue to digital: A Single Patient Record accessible through the NHS App by 2028 will become the “front door” to the NHS, supporting AI-powered diagnostics, medicine management, and care planning. New AI tools being tested on the Federated Data Platform, which connects information across healthcare settings and links siloed sources, which can reduce the time spent on paperwork by 51.7% and allow each doctor to treat 13.4% more patients during a shift.
- From treatment to prevention: The plan aims to create a smoke-free generation, tackle obesity, reduce alcohol harm, and eliminate cervical cancer by 2040 while increasing access and uptake of screening services via the Neighbourhood Health Service and scaling genomic and predictive analytics to support prevention.
Five enabling reforms:
- A new operating model, merging NHS England with DHSC, empowering ICBs as strategic commissioners, and reintroducing earned autonomy for high-performing NHS organisations.
- Enhanced transparency of quality of care, publishing league tables of providers and patient experience measures, revitalising the National Quality Board as the single authority on quality, and implementing AI-led warning systems to identify at-risk services based on clinical data.
- Workforce transformation, focusing on AI-enabled productivity, advanced practice roles, ultra-flexible contracts, and technology to release £13bn worth of staff time.
- Innovation and technology with five “big bets” (AI, data, genomics, robotics, wearables) drawn from the Future State Programme, new Global Institutes, and faster clinical trial and medicine approval pathways.
- Financial sustainability via a value-based approach focused on getting better outcomes for the money we spend and clearing deficits through 2% annual productivity gains, multi-year budgets, and innovative capital investment models, alongside “Patient Power Payments” linking funding to patient experience.
What does this mean?
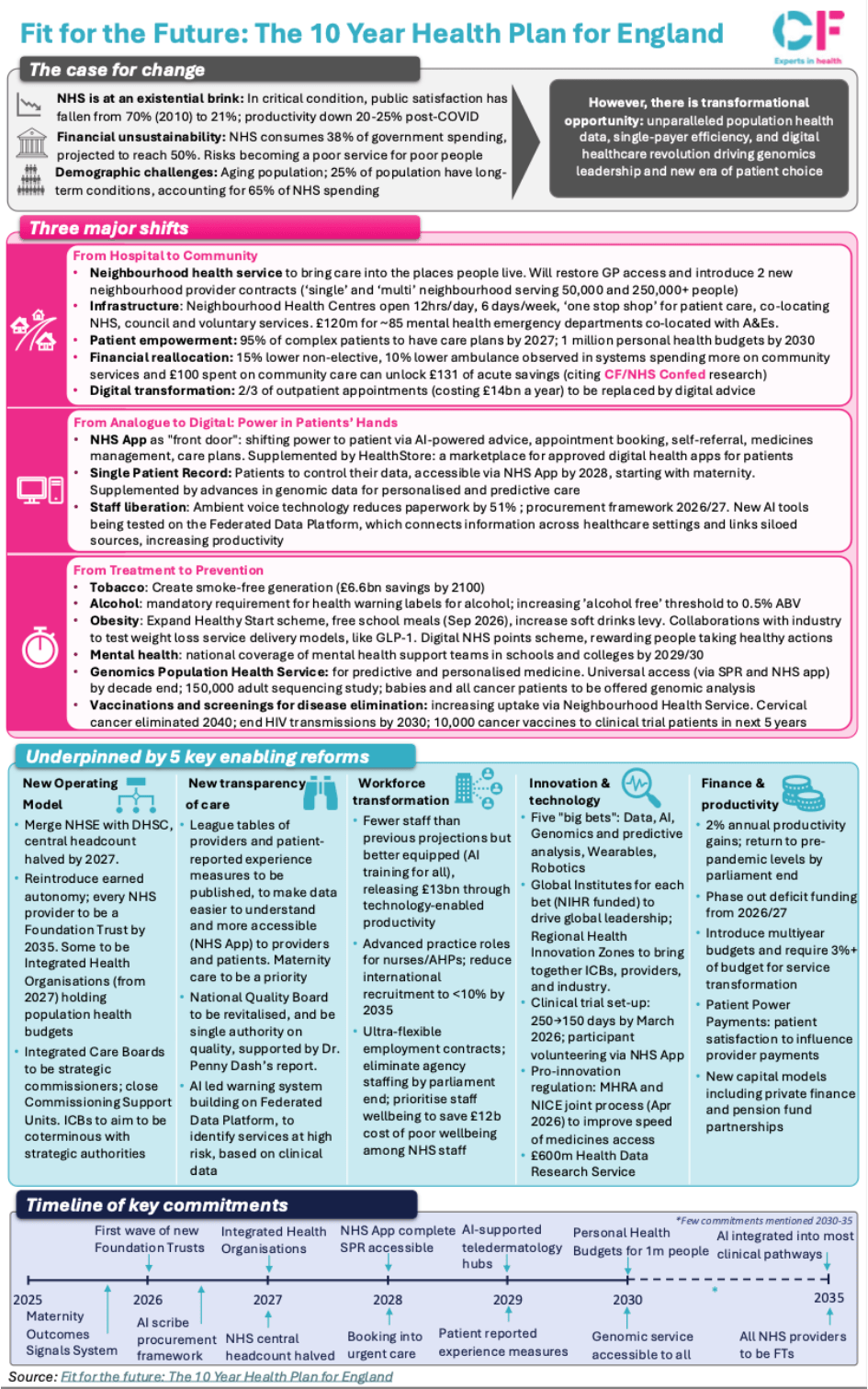
See our snapshot below for a full breakdown of the plan:
Click here to enlarge.
Steps going forward
Success hinges on effective implementation across multiple domains:
- Strengthening the data and digital infrastructure to support the single patient record and genomic analytics.
- Supporting NHS leadership and local systems to adopt new models while maintaining delivery during transition.
- Harnessing AI and automation not only to improve patient care but also to drive the productivity gains necessary for financial sustainability.
In our recent report, Improving productivity, quality and prevention, we highlighted that the NHS’s challenges are deeply linked to its ability to unlock productivity, close quality and care gaps and invest in prevention through better data, technology, and preventative models. The 10-year plan aligns with these imperatives, but its success will hinge on clear prioritisation, robust implementation, and a strong focus on outcomes.
Read the full 10 year plan here. To learn more about our recent reports in support of the 10 year plan see our Value in Health series and Future state Programme report or contact our team.