The COVID-19 pandemic has had a huge impact on healthcare systems around the world, in large part due to the need for capacity to treat COVID cases, which has also had significant effects on non-COVID activity. We previously looked at how the pandemic has affected society, healthcare systems and the life sciences industry. We know that the effects have manifested in different ways across different areas, which is why we are now taking a closer look at how COVID-19 has impacted different patient segments at different stages of the pathway. Specifically, we have mapped out the changes experienced by various patient segments including the mostly healthy and the most at-risk groups (patients with priority acute conditions, cancer, mental health and multiple long-term conditions), against different stages of the pathway (prevalence, access/diagnosis, treatment and post-treatment/recovery).
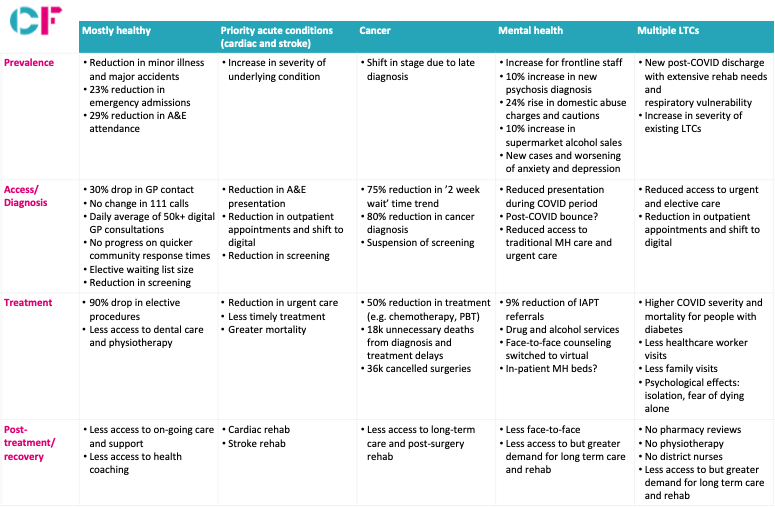
All segments have experienced a reduction in activity, including in emergency admissions, GP contact, screening, elective procedures and access to long-term care and rehabilitation services.
Looking at different patient segments, we find that as expected, older people and patients with long-term conditions have been particularly impacted. Nowhere is this made more evident than in the excess risk of mortality of diabetes and obesity in particular which each independently carry mortality risk of 2.4x relative to those without these conditions. In addition to the higher risk of mortality from COVID itself, with decreased access to primary care, urgent and elective care, they run the risk of exacerbating their existing conditions. The dominant approach to managing the risk present was shielding as vulnerable patients as opposed to managing disease conditions. This is also accompanied by the psychological effects stemming from isolation and the lack of family and healthcare worker visits. Looking ahead it is becoming clear we need to do more to address underlying conditions especially diabetes and obesity and also plan to prioritise these groups for any vaccine once available.
Cancer is also hard hit and could rival COVID deaths. It has experienced major disruptions across the pathway, including the suspension of screening, a significant drop in referrals and diagnosis, reduced chemotherapy and radiotherapy and the cancellation of surgeries. A likely outcome is a shift in stage of diagnosis which means that many patients will be detected late and therefore experience worse outcomes. The number of excess deaths to result from this is estimated to be between 7000 and 36000. It will be urgent to restart the cancer pathways, including getting patients to present their conditions, GPs to refer and then crucially to have sufficient diagnostic capacity in form of kit and staff to support rapid diagnosis. It will also be necessary to consider how to fund cancer services if they need to operate at 50% of normal capacity due to infection prevention control.
Due to the lockdown, isolation, uncertainty and economic repercussions brought on by the pandemic, mental health is emerging as an area of concern, with reported increases in domestic abuse and alcohol consumption. There has been more mixed views anecdotally on anxiety, depression and psychosis. There is a particular concern about the impact on the mental health of front line workers who might be expected to experience consequences of the stress of combatting the virus. This is obviously particularly critical to maintain the resilience of the NHS to any further wave of COVID.
Finally, cardiovascular disease and stroke are also high priority acute conditions that have experienced a substantial slowdown in activity amid the outbreak. Less patients have been presenting in A&E and to outpatient appointments. The likely result is a worsening of their existing conditions leading to worse outcomes and mortality.
In thinking about how to recover from these disruptions to the healthcare system, it is important to consider not only how to clear the backlog of cases most effectively and rapidly, but also how to prevent these disruptions from occurring again in the event of further COVID-19 peaks. This suggests the need to:
- Target recovery efforts in each local area on the most critical patient segments
- Shift our focus from shielding to disease management in COVID secure environments
- Maximise the use of virtual and digital to triage and accelerate cases that need to move forward
- Provide the finances to fund operation at lower levels of utilisation than normal


