The COVID-19 pandemic has put healthcare systems around the world under strain and has in large part monopolised their capacity. Whilst focusing on resources and capacity on fighting the outbreak have been necessary, it has brought some unintended consequences that are likely to have long-term impacts on health and care systems and patient outcomes.
In the UK, a build-up of from weeks of patients staying away from healthcare settings and disrupted health services have created a backlog of elective and non-elective cases that need to be addressed. Cancer is a particular area of concern, as cancer patients are an especially at-risk cohort with an elevated risk of experiencing worse outcomes from COVID-19 [1]. The entire cancer pathway has been disrupted during the outbreak, leading to a major slowdown in diagnosis and treatment activities. This has not been the case in all countries, as some, such as Italy and China, have managed to keep delivering complex radiotherapy and chemotherapy throughout the COVID crisis.[2]
For many patients, cancer treatment has been stopped due to its immunosuppressing effects, however, there are some cancer services such as PBT which has been delayed due to capacity.[3]Indeed, many cancer outpatient visits have been replaced with telephone consultations, and some routine therapy, tests and procedure have been deferred.[1] Screening has also been put on hold as the UK’s cancer screening programmes (breast, bowel and cervical cancers) have been delayed due to outbreak.[4]
Despite the UK government announcing on 27 April 2020, that cancer care would resume, there are multiple factors which have seen both a reduced uptake and a reduction in services. Patients are being assessed to determine whether the risk of bringing them into a hospital environment outweighs the risk of delaying treatment. Services such as endoscopies and scans have had to be reduced as appointment times have had to be increased to do the necessary cleaning and disinfecting to keep the environment safe for both patient and doctor.
Now that the UK has reached the peak number of daily COVID-19 cases, it is imperative to take a closer look at the immediate and long-term impacts of disrupted cancer detection, treatment and the impact on patient outcomes., It is necessary to evaluate what the impact is, in order to work out next steps to address the issues that have arisen.
Impact on cancer activities
Cancer Research UK has observed that every step of the cancer pathway has been disrupted by COVID-19, including, screening, GP referrals, diagnostics, testing and treatment.[5]
Screening
Invitations and follow-up appointments are being delayed for all three of the UK’s cancer screening programmes (breast, bowel, and cervical cancer) due to the COVID-19 pandemic. These screening programmes allow for the early detection of these cancer types before the presentation of symptoms, which can mean a better prognosis for the patient. Now that these programmes have been paused, 200,000 people are no longer being screened every week, and thus a significant number of them are missing the opportunity of an early detection.[5]
Diagnosis
Cancer diagnosis has been significantly disrupted as patients with possible signs of cancer have been staying away from health services due to fear of infection. Whilst GP appointments have been available to patients through virtual consultations, which has been an important transition for the NHS, some GPs are hesitating to send their patients to local hospitals for diagnostic tests out of fear of spreading the virus to patients and staff.
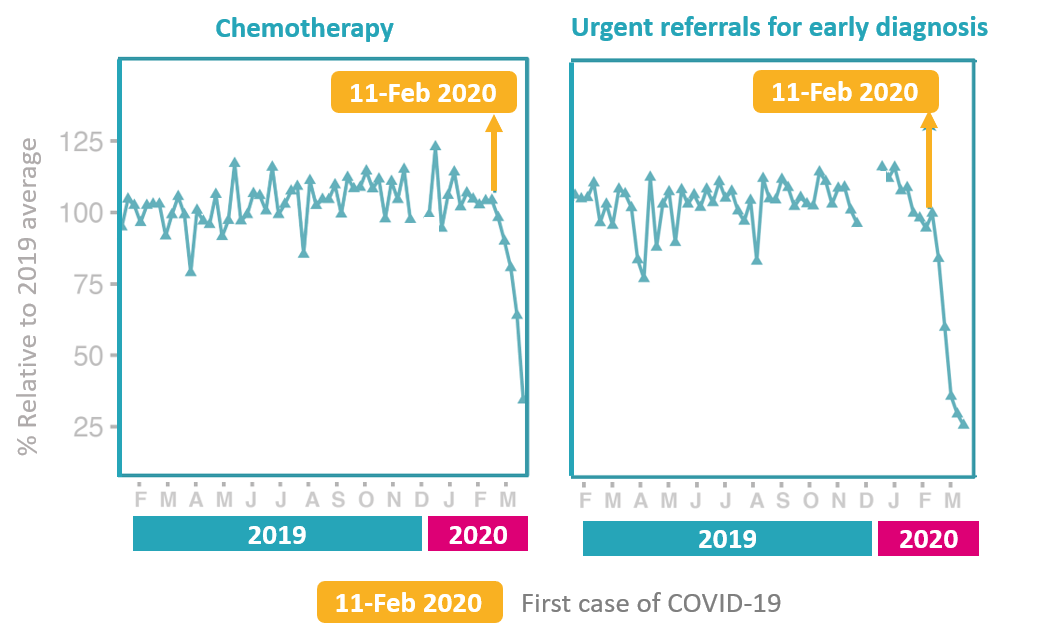
For these reasons, urgent referrals by GPs of people with symptoms of cancer have dropped by 75% compared to usual levels in England. Consequently, more than 2,300 cancer cases are likely to be going undiagnosed every week in the UK, which will lead to a significant build-up of cases.[5]
Treatment
While guidelines from NHS England have insisted that urgent cancer treatment will be unaffected, in practice there are inconsistencies in what treatment is available depending on the region within the UK. Early cancers are being ‘parked’ for 3 months or more, with the chances of curative surgery becoming less likely.[5] A recent study of four hospitals across England has found that chemotherapy attendances have decreased by 60% amid the COVID-19 pandemic.[6]
Patients who usually travel abroad for Proton Beam Therapy have quite sensibly stopped receiving treatment as borders close and flights have been suspended. The Christie Hospital within the UK, which does offer PBT, does not have sufficient capacity to treat everyone. There are other operational centres (North East England, South Wales and Reading) with spare capacity that could be utilized to give PBT treatment to those who would usually travel abroad.[3],[2]
Approximately 36,280 cancer surgeries have been cancelled in the UK, with a 12-week cancellation rate of 28.8%. The NHS estimates an average of £4,000 per surgery, which means that clearing the backlog in cancer operations will cost over £145 million.[7]
Research
Cancer clinical research activities have been slowed down or suspended as efforts have shifted to COVID-19 research. Recruitment of participants and new trials have been put on hold, which will result in significant delays in clinical research and drug development timelines.[1], [5]
Potential impact on patient outcomes
Amid the COVID-19 outbreak, there has been a 75% decrease in ‘two-week wait’ numbers, which means that only 25% of people are being diagnosed compared to usual levels in England. [5] The disruptions to the cancer pathway will likely result in cancer being diagnosed at a later stage. Patients diagnosed at later stages have fewer treatment options and have a worse survival rate.
If the disruptions to the cancer pathway were to mean that people who would have otherwise been diagnosed during the COVID-19 period end up being diagnosed a stage later, then the stage shift in the three biggest cancers will look like this:
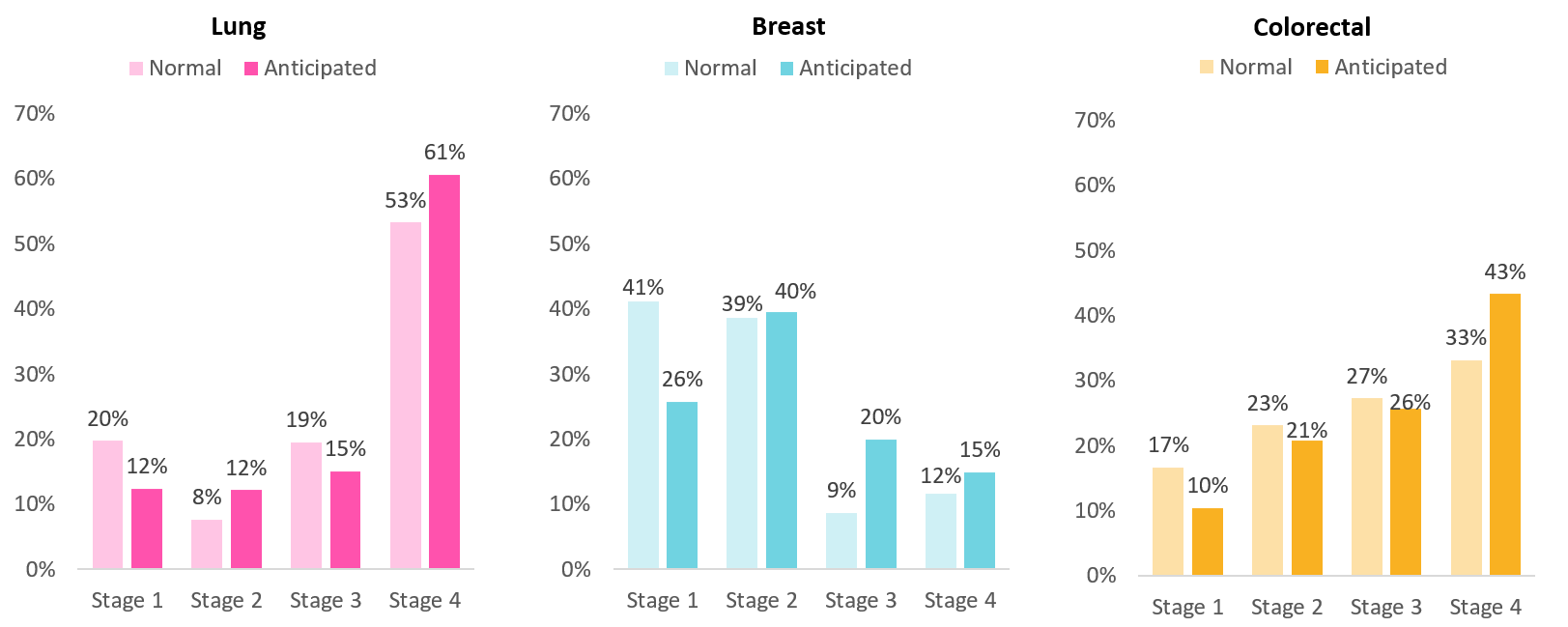
Taking lung cancer as an example, we can see that while in a normal distribution 53% of people with lung cancer are in stage 4, this proportion would go up to 61% in 2020 due to a shift in the stage of diagnosis. Looking at the corresponding five-year survival rate, this implies that more people with lung cancer will only have a 3% chance of survival to 2025. Hence, the increase in patients who are diagnosed at a later stage will most likely result in unnecessary deaths.
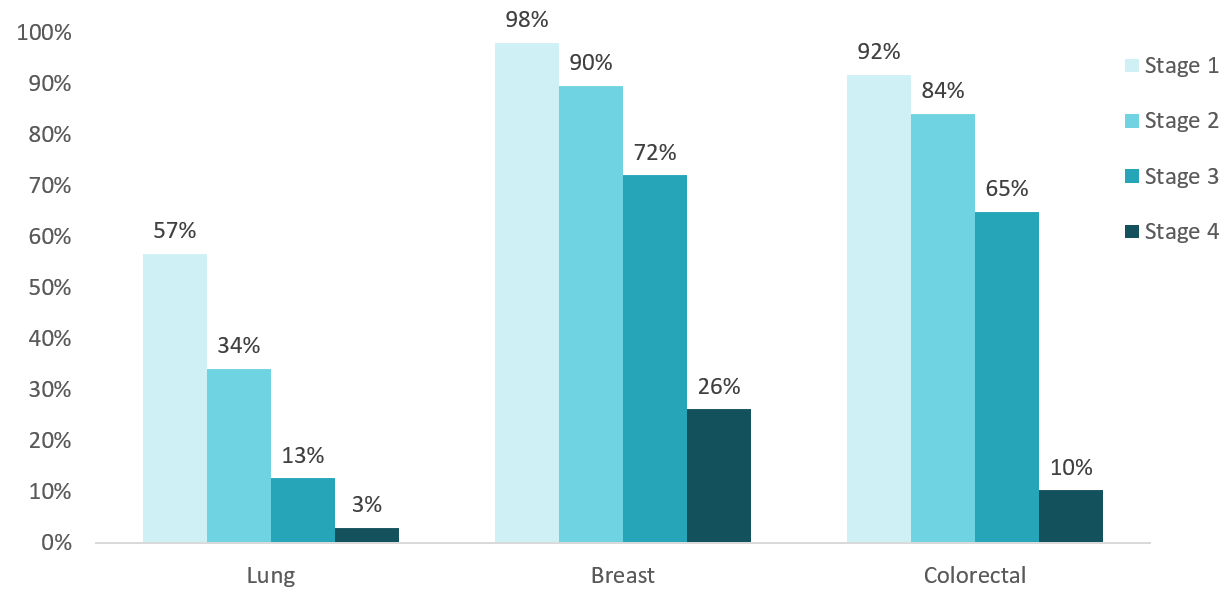
Some researchers have already tried to estimate the additional cancer deaths that will result from this set-back. A recent study done by DATA-CAN in conjunction with University College London, The Royal London Hospital and others has found that there will be somewhere between 7,164 and 35,830 more cancer-related deaths due to the disruption brought on by the COVID-19 pandemic.[6]
What needs to be done
In order to clear the backlog of cancer cases that have been building up for weeks, health and care systems will need to adopt certain measures to ensure safe and efficient delivery of services to lead to optimal outcomes.
Prioritise cases
Patients in need of urgent care need to be identified with the ability to fast-track these cases. The NHS has released a guide for prioritising patients for cancer treatment during the COVID-19 pandemic, which identifies six priorities for chemotherapy and five for radiotherapy.[10],[2] Broadly, the guide gives priority to patients with conditions that are immediately life-threatening or critically unstable, and to interventions that will result in survival gain or improved quality of life.[1]
Use safe sites
To prevent usual services being shut down by COVID-19 treatment, it will be imperative to treat cancer patients in COVID-free sites to protect them from infection. In the event of further COVID-19 peaks, having COVID-free sites will be crucial to prevent more disruption in cancer services and to keep patients safe from infection.
Fortunately, hospitals in 19 areas of England are operating now as ‘cancer hubs’ (e.g., in London, Manchester and Leeds), which have areas which do not treat COVID-19 patients, the space is dedicated for cancer treatment.[11] Instant testing will need to be made available to every patient and staff member at these sites in order to ensure that these sites remain safe for patients and staff.[5]
Make use of private sector capacity
To manage the build-up of cases, the NHS has secured six months of capacity from March 2020? in the private sector which could be used to help provide safe areas to treat cancer patients without increasing the risk of exposure to COVID-19. Furthermore, independent cancer care has sufficient capacity and resources to accommodate thousands of patients.[6]
Encourage patients to use health services
Throughout the COVID pandemic, there has been strong and effective messaging urging people to stay home to prevent the spread of the virus. While this campaign has been necessary to control the outbreak, it has also kept non-COVID patients away from health facilities, including cancer patients. To that effect, the government has launched a campaign to encourage patients with urgent needs and serious conditions to make use of health services, including cancer screening and care.[12] It is essential to carry-on reassuring patients that they can seek treatment.
References:
[1] The Lancet, Effect of the COVID-19 pandemic on cancer treatment and research: https://www.thelancet.com/journals/lanhae/article/PIIS2352-3026(20)30123-X/fulltext
[2] Financial Times, How to avoid rationing urgent healthcare during the Covid-19 outbreak: https://www.ft.com/content/30448a84-736d-11ea-90ce-5fb6c07a27f2
[3] Oncology Central, The potential impact of COVID-19 on cancer mortality in the UK: https://www.oncology-central.com/in-focus/in-focus-coronavirus/the-potential-impact-of-covid-19-on-cancer-mortality-in-the-uk/
[4] Cancer Research UK, Cancer screening and coronavirus (COVID-19): https://www.cancerresearchuk.org/about-cancer/cancer-in-general/coronavirus/cancer-screening
[5] Cancer Research UK, How coronavirus is impacting cancer services in the UK: https://scienceblog.cancerresearchuk.org/2020/04/21/how-coronavirus-is-impacting-cancer-services-in-the-uk/
[6] Researchgate, Estimating excess mortality in people with cancer and multimorbidity in the COVID-19 emergency: https://www.researchgate.net/publication/340984562_Estimating_excess_mortality_in_people_with_cancer_and_multimorbidity_in_the_COVID-19_emergency
[7] BJSS Journals, Elective surgery cancellations due to COVID-10 pandemic: global predictive modelling to inform surgical recovery plans: https://bjssjournals.onlinelibrary.wiley.com/doi/abs/10.1002/bjs.11746
[8] NCRAS, Survival by stage: http://www.ncin.org.uk/publications/survival_by_stage
[9] Office for National Statistics, Cancer survival in England, adults diagnosed: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/datasets/cancersurvivalratescancersurvivalinenglandadultsdiagnosed
[10] NHS England, Clinical guide for the management of noncoronavirus patients requiring acute treatment: Cancer: https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/specialty-guide-acute-treatment-cancer-23-march-2020.pdf
[11] The Guardian, Coronavirus crisis could lead to 18,000 more cancer deaths, experts warn: https://www.theguardian.com/society/2020/apr/29/extra-18000-cancer-patients-in-england-could-die-in-next-year-study
[12] The Guardian, England campaign targets seriously ill patients avoiding hospitals: https://www.theguardian.com/world/2020/apr/25/england-campaign-targets-seriously-ill-patients-avoiding-hospitals


