The COVID-19 crisis has caused a dramatic shift in how care is delivered. All forms of health activity experienced dramatic reduction and the activity that did continue shifted, almost instantly, to virtual. The latter has been pointed to all as the silver lining of the COVID-19 crisis and the mantra “digital by default” must be maintained with “no going back”.
There have been anecdotal stories of 80% plus conversion from in-person to virtual contacts. This is perhaps best exemplified by some of the digital providers and the traction they have got nearly overnight. For example, DrDoctor, released a free COVID-19 toolkit for NHS Trusts with video consultation software, broadcast messaging and COVID-19 symptom assessments, reaching more than 161,000 patients in the first three days following release. AskmyGP’s data shows a movement from approximately 50,000 patient requests per week pre-COVID-19 to more than 100,000 requests per week during COVID-19 for primary care consultations that come in digitally from their platform.[1] These are stories to be celebrated. They may not yet be universally representative as are examples of digital providers.
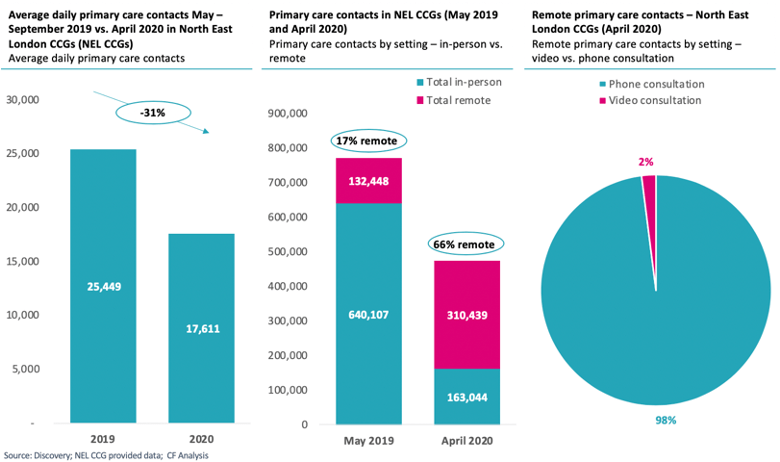
We worked with North East London (NEL) to access agregated data across the whole ICS to understand what has happened. This analysis of primary care data (see Fig. 1) highlights how COVID-19 caused a dramatic shift in the provision of primary care:
- First, there was a sharp decrease of overall primary care contacts. Average daily primary care contacts dropped by 31% as a result of COVID-19. Before COVID-19, there were 25,500 primary care contacts per day, during the response to COVID-19, this fell to 17,500.
- Second, there has also been a 4x increase in the share of remote appointments in primary care when compared to the previous year.[2] In April 2020, 66% of primary care contacts were delivered remotely compared to just 17% in May 2019. This shows how rapidly primary care employed remote technologies as it adapted in to COVID-19.
- Third, despite such a high proportion of care being delivered remotely, just 2% of remote contacts were delivered via video links, the rest were phone consultations.
This remains a major transformation—just a slightly different one than we have heard about. It has kept people safe, been more convenient for patients, and enabled efficient triage and discussion by telephone. It has demonstrated that there is no reason for an in-person consultation in many cases.
This therefore means we need to maintain “virtual by default” as undoubtedly better for patients and healthcare professionals. This will be particularly important over the coming months as primary care encounters a likely ‘bounce back’ from the supressed COVID period, significantly stretching current capacity.
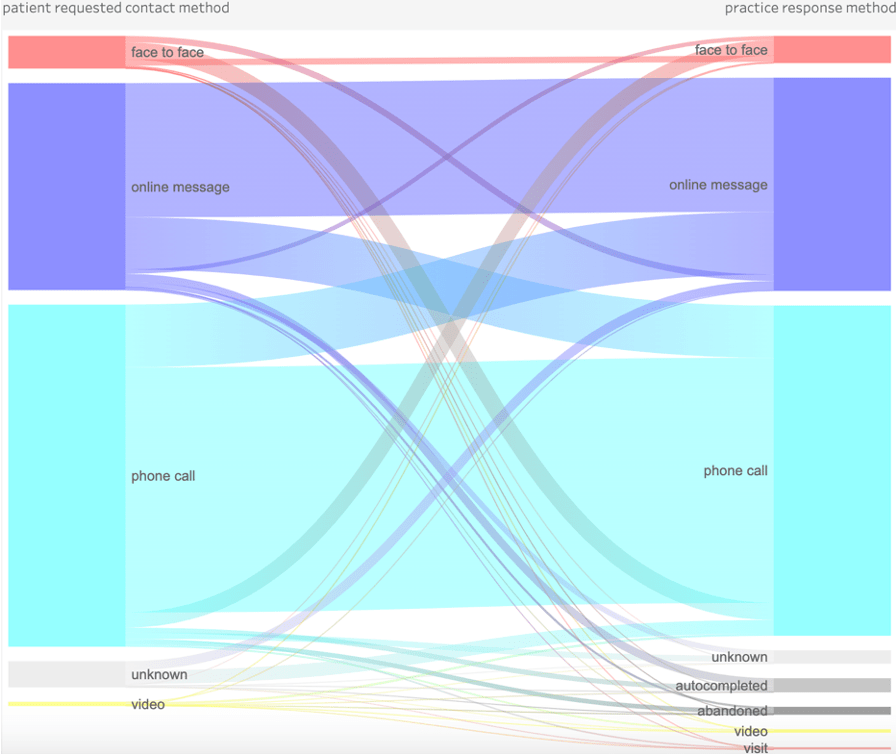
Beyond telephone and video, online messaging is another useful tool with room for development. While the NHS has yet to fully adopt instant messaging technologies, these technologies show considerable promise in other settings. For example, askmyGP employs messaging technologies to good effect, with many of their patients using online messaging as their default communication method with their GP (see Figure 2).
Having shifted from physical appointments to virtual, we need to embrace the progress made and push further to make use of true digital interactions—to determine the urgency and nature of need, respond as conveniently as desired (whether phone, video, text, etc), and in some cases (such as routine diagnostics or prescription refills) consider if an appointment is needed at all.
Digital technologies can be employed at many points along the patient journey – here is an initial list to consider:
- Making initial contact – enabling triage and scheduling further contact (whether by phone, video or text)
- Providing further detail and enabling patients to share images with clinicians
- Communicating short bits of information via text
- Capturing and sharing test results via digital platforms
- Prescription refill request and processing
- Determining if onward referral is needed and communicating this message to patients
There is an urgent need to learn from areas and examples that have made progress to digital. We would love to hear your stories about this in whatever sector of healthcare they happen in – from shielding the vulnerable, to supporting the frail elderly , to video conferencing for GPs and consultants and supporting remote diagnostics, consultations for maternity and MSK, and access to online support for mental health.
[1]AskmyGP Live Analytics, https://askmygp.uk/live/
[2] NHS Digital, Appointments in General Practice March 2020: https://digital.nhs.uk/data-and-information/publications/statistical/appointments-in-general-practice/march-2020


