Preparing for delivering the vaccine
So there is finally light at the end of the tunnel with very promising findings announced in the last week for two Covid vaccines from Pfizer and Moderna. This is the result of tremendous innovation in the life sciences industry with two totally different mechanisms developed both in comparatively lightning speed. It has been supported by a regulatory and procurement approach that has supported multiple competing solutions to be able to launch whichever showed greatest promise, through unprecedented collaborative working across the regulating bodies. A sensible prioritisation for access to the vaccine has been set out, highlighting care home residents and workers, frontline staff, and essentially the population by age and vulnerability.
It’s now up to the National Health Service to rapidly roll this out to the people who need it the most, as fast as possible. With a national universal health service, we are well placed to do this, but it will undoubtedly be challenging.
We foresee three key areas that must be rapidly thought through for this to be successful. How to reach the right patients, how a combined national and local delivery model will work and how to connect the system together? Collaboration between primary care, acute NHS providers, care homes and Local Authorities is going to be crucial to overcoming these challenges:
1. How do we reach the right patients?
- What is the prioritisation by cohort in each local area?
- How in practice does the prioritisation of frontline health and care staff sit alongside the prioritisation of successive waves of patient cohorts, especially when not all staff are resident in a local place? Given more than 1m hospital staff and several hundred thousand care home staff, these questions are significant in the face of limited vaccination supply
- How is uptake maximised? How is support for vaccination encouraged? How can we build trust and demonstrate safety to drive uptake?
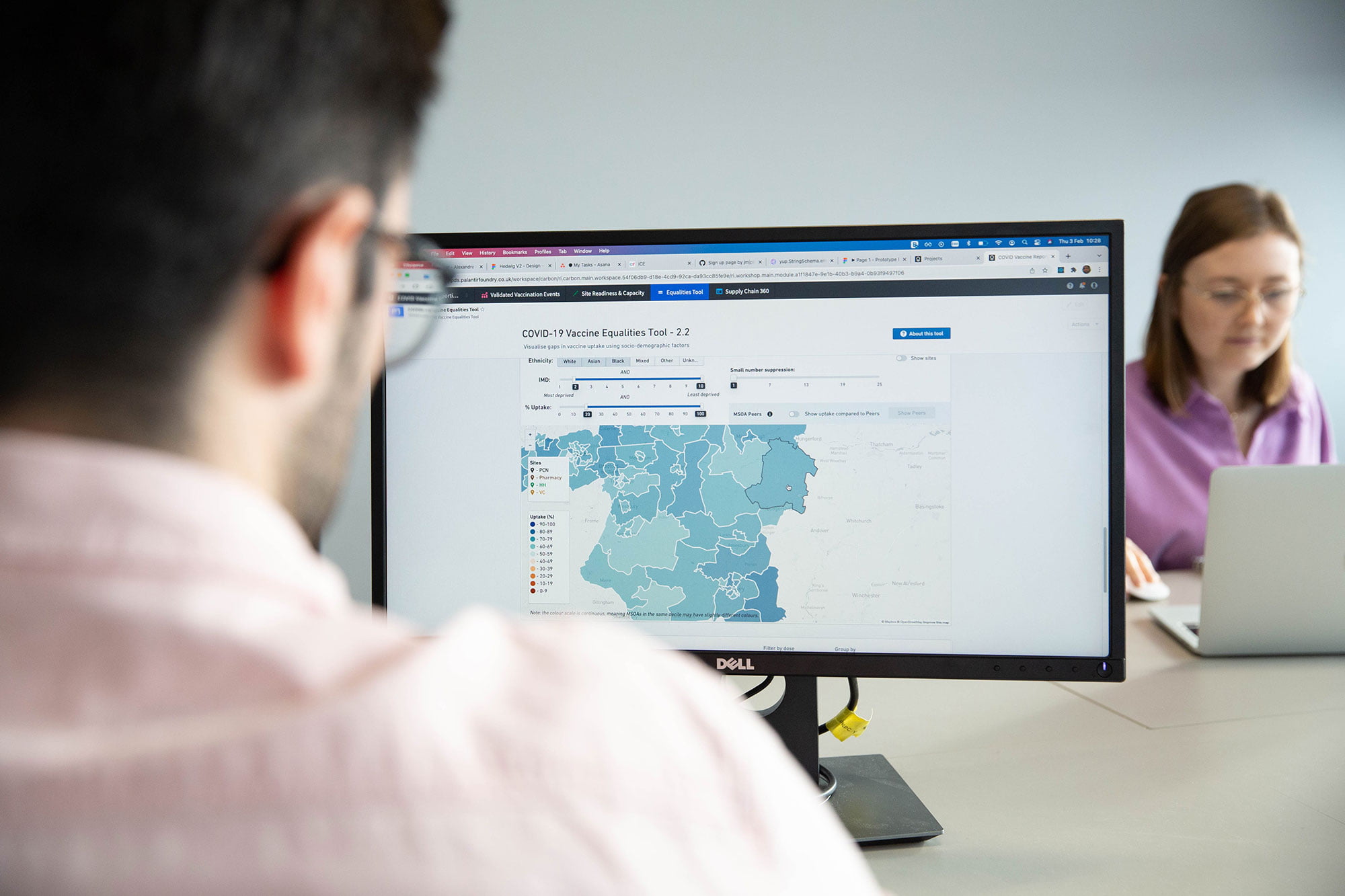
- How do we ensure there is no health inequality in uptake of vaccine especially from deprived and ethnic communities who have suffered greatly already? How do we ensure hard to reach groups are not left behind?
2. What is the best delivery model?
- Who will have accountability for delivery to each segment within each place? Will this be NHS England regional offices, or ICS and Primary Care Networks (PCN), or providers (care homes, hospitals, GP practices)?
- What will the delivery model to reach staff and patients be? Primary care and pharmacies are the traditional means for flu vaccination and given that are the natural leads for this work. Care homes are typically covered by specific GP practices and hospitals have taken responsibility for their own staff. However, the Secretary of State has spoken of mass vaccination and roving vaccination teams, which is not how flu works. And whilst hospitals have vaccinated staff for flu they have not worried about cold supply chain or recording details.
- How are vaccines distributed to where they are needed? The answer depends on the cohorts prioritised and delivery model, but also needs to recognise the different vaccine storage requirements (e.g. down to -70C) and the need to maximise use of doses and vials within time limits of effectiveness?
- How is waste minimised? How do we make sure patients turn up as booked and minimise “Did Not Attend” (DNA)? How do we ensure that the limits of effectiveness in temperature control of the vaccine does not result in waste?
- How will the physical capacity needed for vaccination (with social distancing and COVID-secure measures) be managed to optimise both vaccine throughput and maintain primary care activity in wide range of settings?
- How will workforce needed be accessed so that it is sufficient to deliver vaccines as fast as supply becomes available without depressing needed primary care capacity for cancer, cardiovascular, chronic conditions and mental health? If additional workforce are accessed (from pharmacists, community staff, retired health professionals, volunteers) how will they be integrated to support vaccination programmes?
- How will payments be made to primary care for carrying out vaccination? And what will be the burden of recording and reporting in order to enable this to happen?
3. How to connect the system together?
- Who will invite patients and staff and how will they do it? Will the invitation come from the GP, or the local NHS? By email, text, letter, call, knock on the door? Where will they go for it? How will any confusion over the appropriate channel be avoided in overlap between staff and patients?
- How will patients and staff book an appointment? With their employer for staff and via primary care practice, or PCN? Or will a national or regional booking system be created?
- How does the NHS ensure a single view of the truth of who has been vaccinated and where the gaps are without adding extra layers of assurance requirements to primary care? How is data captured in patient record if vaccination happens outside of primary care?
These are difficult questions to answer which will require learning from both flu vaccination programmes and from recent Covid national and regional planning exercises. The new primary care networks are well placed to lead much of this but will need regional and national support. It will need collaboration in each local place with providers (hospital and care homes especially) and Local Authorities to plan, communicate and deliver. We recognise that everyone is going to be working extremely hard on this. Our escape from lockdown depends on this.
About the authors
Dr Simon Munk
Simon, Consultant at CF brings medical and operational expertise across our projects in acute, mental health and children’s community services.
Will Browne
Will, healthcare analytics and product development lead at CF. Will combines consultancy experience with data science expertise to develop pragmatic solutions to real-world problems in healthcare.
Dr Zahra Safarfashandi
Zahra, Senior Manager at CF is a clinician and experienced healthcare management consultant who specialises in leading healthcare transformation programmes.
Ben Richardson
Ben is a co-founder of CF and leader of the company’s work in life sciences and healthcare analytics.