A comprehensive review commissioned by the Department of Health and Social Care has revealed a “cluttered landscape” of patient safety organisations that are duplicating efforts, overwhelming NHS staff with recommendations, and failing to deliver proportionate improvements despite £160 million annual investment.
The review, led by Penny Dash, examined six key organisations established to assure or improve care safety, including the Care Quality Commission (CQC), Health Services Safety Investigations Body (HSSIB), and the Patient Safety Commissioner. Its findings paint a picture of a system that has grown reactively rather than strategically, with concerning gaps in effectiveness.
The scale of the problem
While the UK has invested heavily in patient safety infrastructure over the past decade, international comparisons suggest that if the UK had performed at the level of the top 10% of OECD countries in 2022, there could have been 780 fewer deaths per year due to unsafe care.
But the problem extends far beyond safety incidents. In 2022, there were 125,600 avoidable deaths out of 576,000 total deaths – around one in five of all deaths. The variations in care quality are stark: only 54% of cancers are diagnosed at treatable early stages, diabetes care ranges from 62% receiving recommended treatment down to just 1.8% in some GP practices, over 35% of those living with dementia are undiagnosed and just 6% of eligible patients currently receive treatment, as highlighted in CF’s recent Value in Health series.
Of particular concern is the disconnect between investment and outcomes. The review found that despite a 34% increase in full-time equivalent nurses and 37% increase in doctors in acute hospitals between 2013-2024, occupied bed days increased by only 3% and weighted activity by 23%. This suggests significant inefficiencies in how resources are being deployed.
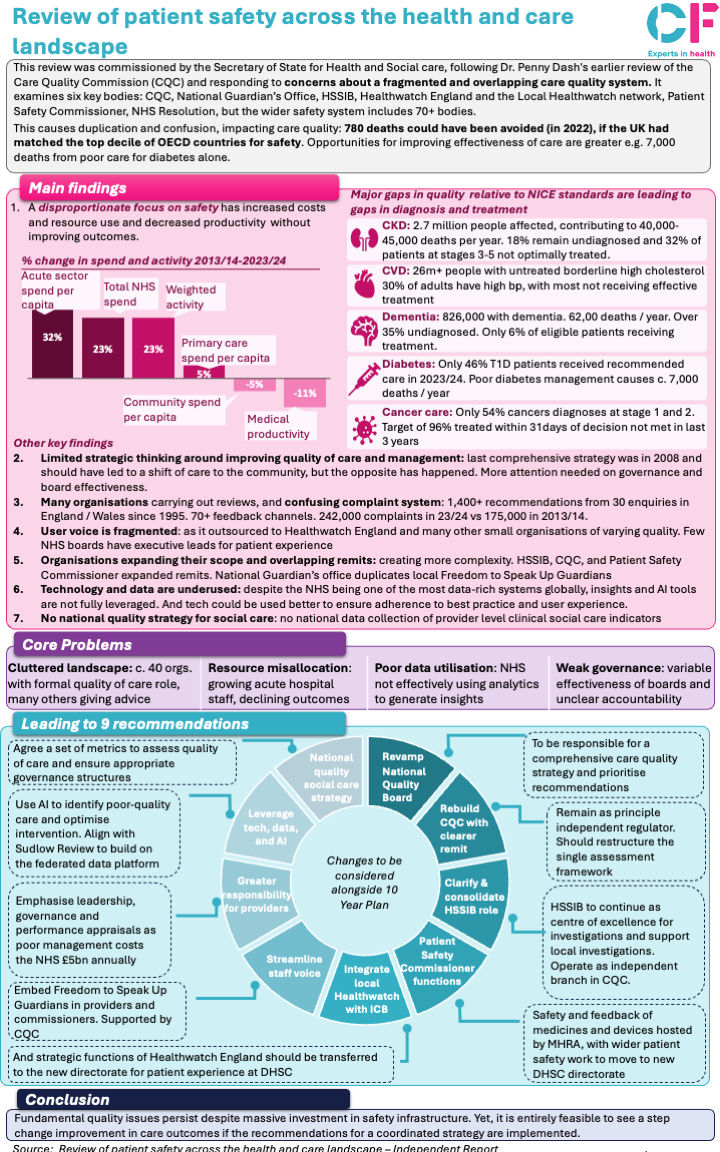
Take a look at our snapshot below that summarises the 10 key findings and recommendations from the Dash Review:
Click to enlarge.
The path forward
The review represents a rare moment of strategic thinking about patient safety infrastructure. Its central message is clear: the current system of reactive organisation-creation following high-profile failures has created more bureaucracy than improvement. Instead, the focus should return to supporting commissioners and providers to deliver high-quality care through better governance, strategic coordination, and intelligent use of technology.
The financial implications are significant. The review estimates that poor management alone costs the NHS over £5 billion annually, equivalent to 330,000 quality-adjusted life years. With productivity in acute hospitals having declined by 8% since 2019-20, representing around £6 billion per year, the case for reform is compelling.
As the government develops its 10 Year Health Plan this review provides a roadmap for creating a more coherent, effective patient safety system. The question now is whether the political will exists to implement these fundamental changes and resist the temptation to create yet more organisations when the next safety crisis emerges.
The full review is available here.
To learn more about this snapshot, contact our Health Systems team today.