Primary care networks are now typically serving natural communities of around 30,000 to 50,000 which is leaving Clinical Leaders wondering how they can best meet the needs of their community whilst serving the Long-Term Plan
While there are high expectations for the new primary care networks, many network clinical directors feel quite daunted by their new roles. The new Primary Care Networks can be serving natural communities of around 30,000 to 50,000 patients, all of whom have differing needs and will use their PCN in a multitude of ways. New clinical leaders have the challenge of ensuring that their networks meet the needs of not just the Long-Term Plan and the local commissioners but most importantly their local community.
Primary Care Networks are not the only health care system to face these challenges, and we have found great success with taking a population health management approach, to identify which patient groups could most benefit from “integrated” care and support.
Using the 3×3 grid approach for Primary Care Networks
We find the 3×3 grid below a useful tool for considering the needs of different groups of people. The grid helps practitioners identify which of their patients would require a different sort of care model.
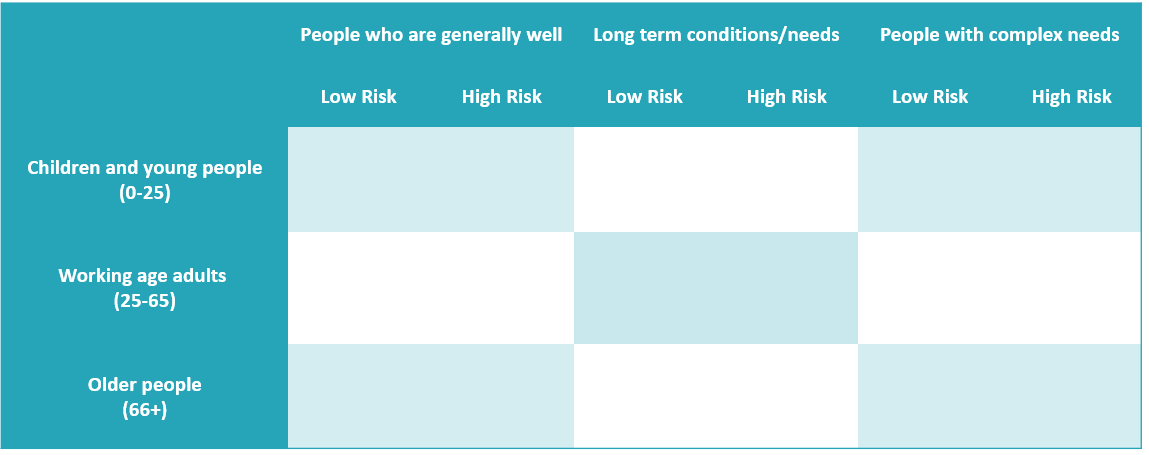
Patients who are placed in the “generally well” or “long term conditions / long term needs” columns are well managed by their GP and practice nurse, with some support from the wider practice-based team and on occasion from hospital or community services.
In contrast, it is the people in the “Complexity of Long-Term Conditions and/or disability” column, who particularly require a different sort of care model. Patients who are placed in this column generally encompass those with a complex mix of physical, emotional, and social care needs, who may also have functional impairment or disability. This group of patients is generally small, for example, frail older patients typically account for 2-3% of patients/100-1500 in a typical Primary Care Network. They will include:
- Children with complex needs and disability
- Frail older adults
- Adults with severe and enduring mental health, drug and alcohol and social challenges.
Evidence (Ham et al, 2011) suggests these patients specifically require holistic, coordinated, joint up, personalised care with a high degree of continuity if their health, wellbeing and independence is to be maximised.
Models of ‘total care’
Patients who sit in the right-hand column of the 3×3 grid, have very differing needs. Models of “total care” for people with complex needs, rather than disease-based models and pathways is helpful. Working at scale within a Primary Care Network enables patients’ access to advice and active support and specialist management.
For example, working within a Primary Care Network gives patients and their carers better and faster access to; palliative care professionals, community care staff, secondary care clinicians, specialist mental health professionals, local community assets (such as voluntary sector services). It allows this support to be provided in a way which makes the best use of primary care and health and care partners’ financial and staffing resources.
The seven-step approach
Taking such a population health management approach, allows you to consider which population groups would most benefit from MDT working; it typically involves 7 steps:
- Gain local buy-in: Engage colleagues in the primary care network, the community themselves and wider stakeholders in considering the value of focussing the network around the care and support needs of and model of care required for particular groups of people.
- Consider the care needs of different patient groups: Use the 3×3 grid as above to understand the needs and number/ proportions of people in a network in the nine different boxes. This relies on working with data colleagues to collect the required data from your primary care system (and ideally patient-level linked data set).
- Understand where outcomes are poor: Review the data to understand which groups of people currently have poor outcomes and where joint-up MDT working could be better for patients and for the staff working in different services. Agree with stakeholders and partners across your network which specific groups of patients to initially focus on.
- Improve services and support: Review what support and services these patients currently receive for their range of health and care needs and consider how this could be improved. Review the evidence base for types of intervention which improve care and outcome for people with these needs. Specifically, consider what support could be provided by a multi-disciplinary team working at the primary care network level.
- Join up working: Consider what can be done to support joint working across professionals for these people, what “care functions” are required. This is likely to include care coordination/case management, care and support planning, rapid response, joint training and support for professionals and use of trusted assessor models where any one of the MDT carries out an assessment of holistic needs on behalf of the MDT.
- Address barriers: Consider the current barriers to delivering joint up care for these people. This frequently includes a lack of trust between professionals and challenges sharing data and accessing patient records between organisations. Consider what can be done across the network in the local context to overcome these challenges. How can the STP/ ICS/ CCG help support this?
- Measure impact: Put in data collection mechanisms to measure the impact of better, joined-up care for these people. Measuring whether these patients with complex needs are more likely to achieve their priorities and have a seamless experience of care can be a great start. Being clear what outcomes are being aimed for, whether this is reducing emergency hospital admissions or reducing failed discharges is vital so that success can be measured against these. Use data and feedback to refine the model of care.


