On 12th November 2019, CF partnered with IPPR to host the State of Care conference which saw speakers from across the health system. Lord Darzi kicked off with a keynote on the state of play since the creation of the Long-Term Plan, specifically touching on workforce demands, the use of digital in healthcare and rounded off with the need for the UK to become early adopters and drive forwards innovation.
I was asked to join the second Panel, “Realising the Frontier NHS”, I was joined by Hilary Hutton-Squire, General Manager and Vice President, Gilead (UK & IE) and Nick Kirby, Managing Director, Shelford Group.
For those who weren’t able to join us, you can find my talk and slides below.
The health sector is blessed with innovators. Every day, people with all sorts of professional backgrounds push at the boundaries of what is possible.
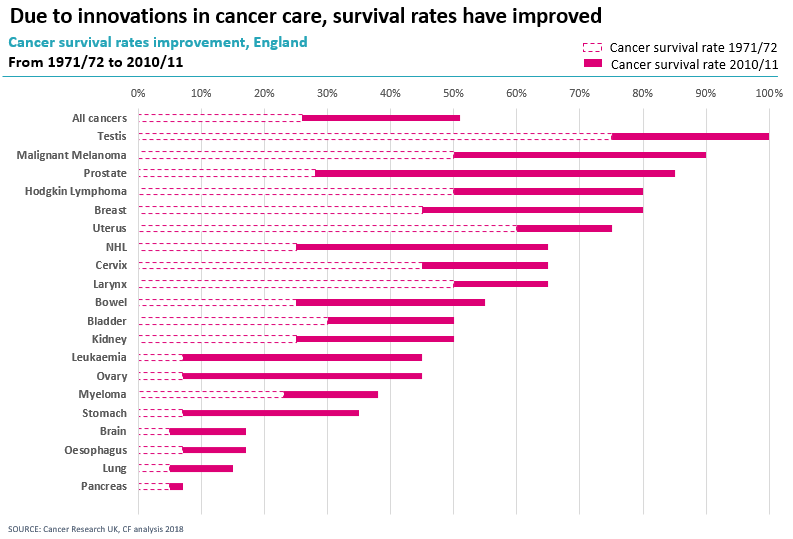
Cancer is a disease that 1 in 2 of us will have to deal with in our lifetimes. Over the last 30 years, we have seen tremendous improvement in survival outcomes. Survival rates have almost doubled, which is in part due to treatment personalisation, methods of earlier detection and new treatment breakthroughs.
The results are impressive, and survival rates can still improve as we continue to innovate cancer treatment.
But what I really want to talk to you about is embracing and adopting the innovations – it’s where we lag behind.
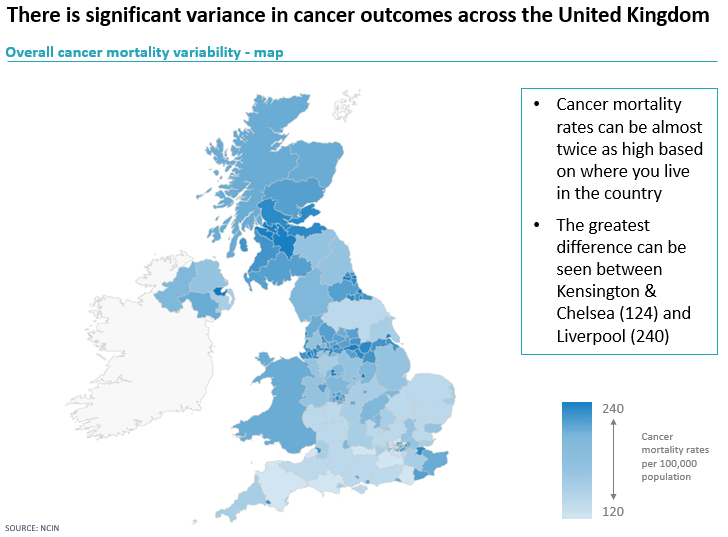
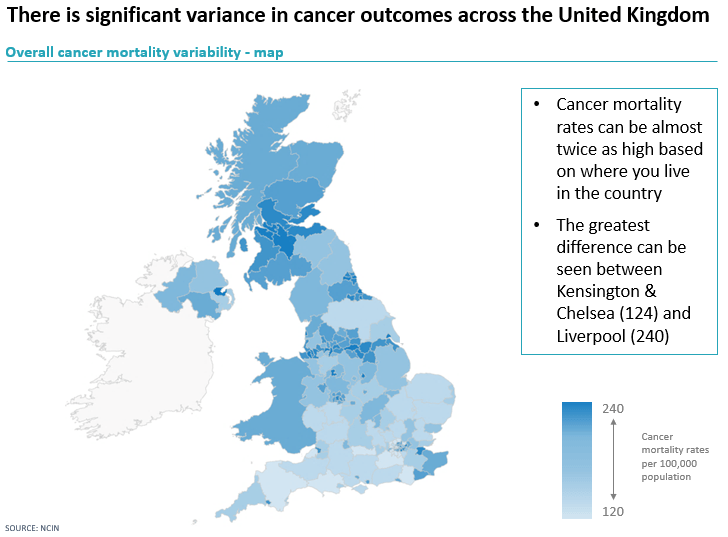
Underlying those survival rates is a significant variation in outcomes, we looked at the latest mortality statistics of all cancers in the UK from NCIN, as you can see in the map the mortality rates massively vary depending on the local health system. If you are diagnosed with cancer in Kensington and Chelsea you are twice as likely to survive than if you live in Liverpool, which is not acceptable. The NHS has seven principles; two of which are ‘equality of geographical access and outcome’ and ‘equality of standards of care’. It is clear there are still a lot of changes that need to be made.
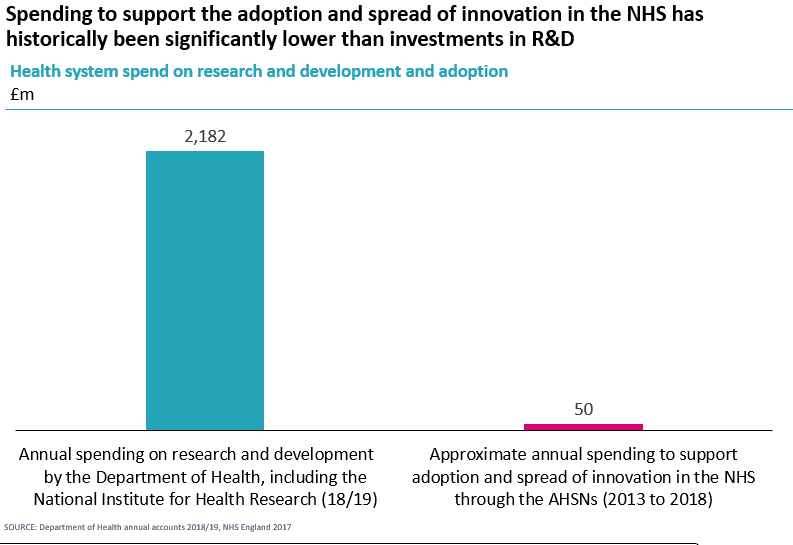
Why is the system struggling? Let’s look at investment.
By looking at the Department of Health accounts from 18/19, we see the stark difference in funds allocated to research and development in the Department of Health is forty times greater than the investment in supporting the adoption and spread of innovation in the NHS through the AHSNs. AHSNs were the delivery mechanism for diffusion. Arguably they haven’t been backed sufficiently to make this a reality.
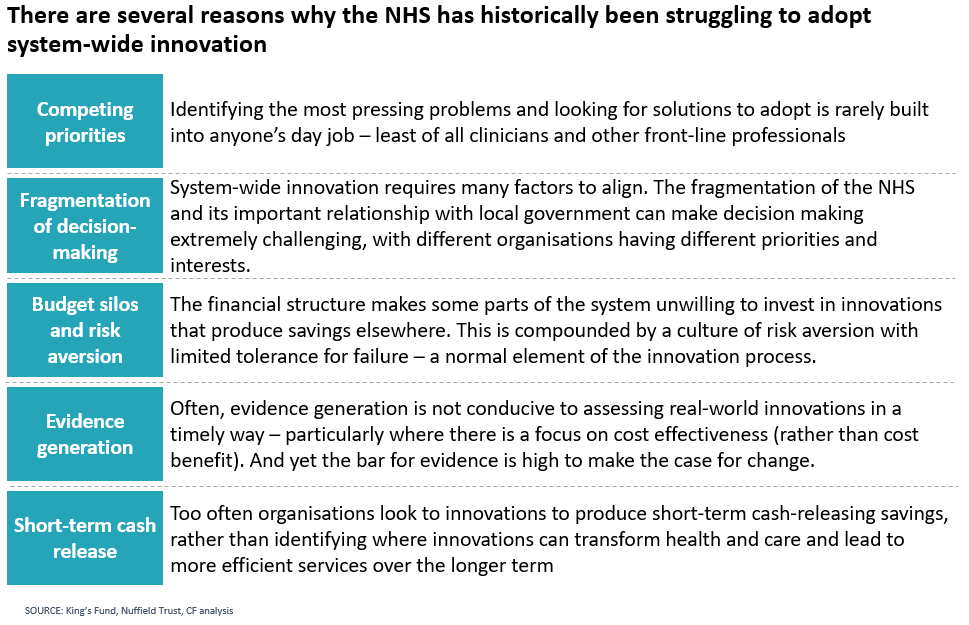
But there are more issues at play.
The current health system is risk-averse, but in innovation, you have to take risks; you’ve got to fail fast and quick. It is necessary to tolerate failure if you are going to innovate, you might get it wrong as often as you get it right in order to push forward boundaries. However, we really cannot tolerate failure in the healthcare sector, there isn’t the flexibility to do it in the workforce and arguably there isn’t the financial flexibility either. It is imperative to capture the evidence required to build a powerful case for change for organisations, in order to adopt innovation.
As a leader in the NHS and as an advisor to many healthcare systems, I have worked on programmes of adoption. Over the course of my career to date, I have learnt many things on how we must and can make a difference in health and care systems.
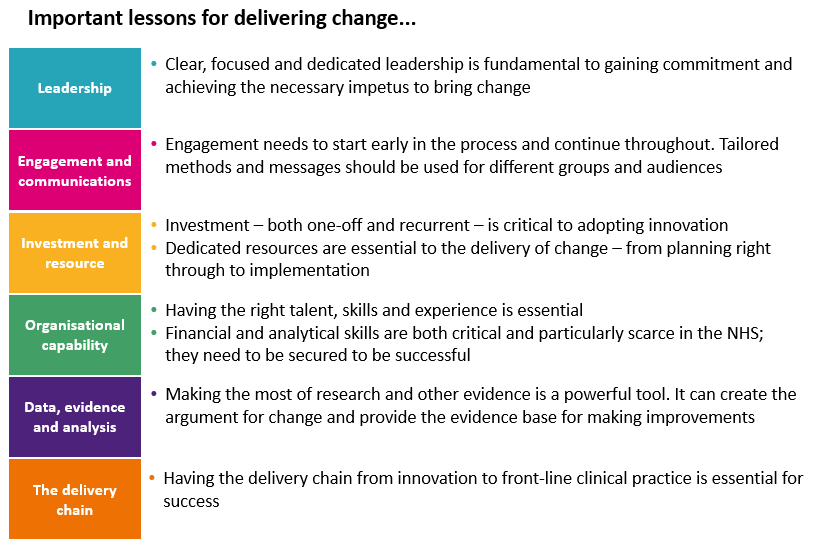
In the health and care sector, innovation can be stifled by the lack of focus. When looking at some responses on how to improve health and care systems, there is no prioritisation, often just long lists of vital changes needed to be actioned. To try and change everything at once is to change nothing. To adopt, nurture and deliver innovation in the NHS, clear prioritisation is needed. If you want to make changes, you’ve got to make choices.