To avoid dropping off a financial cliff within the next five years, there is a consensus growing that the NHS needs to be simultaneously preventing demand, meeting demand in the correct setting of care and then ensuring this demand is met with productive services. In terms of meeting demand in the correct setting of care, it is relatively well recognised that rebalancing care towards community service provision could release a significant opportunity in the NHS.
Currently, popular solutions to this include new models of care, accountable care organisations and population health management; ideas that are all relatively new to the NHS. However, regardless of organisational forms, I believe there are a number of steps that are fundamentally necessary to rebalance services. The steps are to gather data that allows demand in different settings to be compared on a like for like basis and then to engage clinicians to agree how capacity can meet this demand. What follows is a concrete example of such an opportunity in intermediate care and how it could be realised.
Intermediate care aims to allow people to recover their independence and is provided by community services with over 50% of referrals coming from acute hospitals and GPs. The figure below is adapted from the report of the national audit of intermediate care (NAIC) 2017, I have pulled some key figures comparing bed-based and home-based care services.
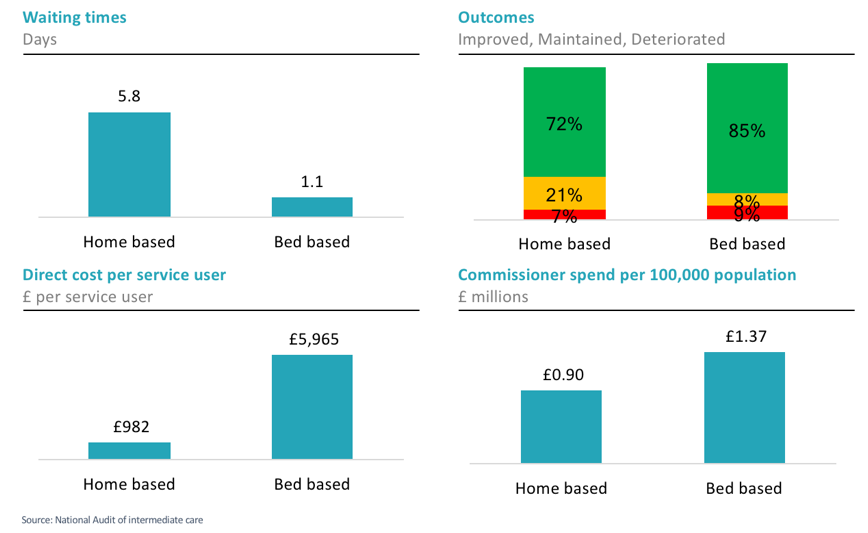
Look at the charts on the left. Wait, 5.8 days wait-time for a referral? Think about this from a purely financial perspective, if a person is waiting in an acute hospital bed at a cost of £250 per day, they will have cost nearly £1,500 while they are waiting for a service that costs £982 on average. For the acute provider with the patient waiting, they can save nearly £1250 by referring the same patient to bed based services with a 1.1 day wait instead of 5.8, yet as we can see, this referral will cost the commissioners £5,000 more.
A series of bed audits across England found 30% of acute beds were occupied by people medically fit to leave for reasons like the lack of available intermediate care. Nationally this is over 20,000 beds which at a cost of £250/bed day is a gross opportunity of £1.8 billion or 2.6% of the c£70 billion spent on acute care (Andrews et al, 2017). Not to mention the harm caused to patients (often frail) spending an unnecessary time lying in a bed becoming deconditioned.
To an outside observer, it seems a compelling case to increase significantly the provision of home-based intermediate care, but to do so requires money that would have to come from a different part of the system. The current system of bilateral contracts means it is very difficult to move money from acute providers to intermediate care as discussed above using contracts alone, yet it could clearly be done without necessarily changing the model of care.
My suggested approach for realising this opportunity is as follows:
1. Clinical audit: The NAIC audit uses a Modified Barthel score for bed-based care and a Sunderland score for home-based care, yet both of these have a number of similar elements measuring dependency. Develop with local clinicians a single index that could be used to measure dependency across bed-based and home-based care and use this in a clinical audit across intermediate care as well as medically fit patients in the acute setting. This could be pre-informed by a mapping of the two existing scores and reanalysis of NAIC data
2. Analyse the data to produce an understanding of current demand and how it is being met, example analyses would be:
- The curve of cost against dependency by setting
- The change in dependency over time by setting
3. Share the analysis transparently with clinicians in provider organisations and ask them to reach a consensus on what demand should be met in which settings. Then agree on a qualified referral process and minimum required service standards (e.g <1 day wait time for home-based services)
4. Model the new capacity in finance and workforce terms and iterate with clinicians if necessary
5. Agree on an implementation plan and how to contract for the modelled activity.
6. If the above sounds difficult, that’s because it is. Moving to accountable care organisations won’t change the fact that we currently don’t have a view of how different needs are being met in different settings. There is no magic bullet for this and as always, the first step should be to get clinicians engaged.




