In the first of our two-part series on realising NHS efficiencies through community healthcare, we look at how improvements to community services data can result in more efficient investment.
 Our previous analysis and reports have highlighted the potential of community services to reduce the burden on acute care, making the entire healthcare system more efficient and productive. However, to fully harness this potential, we must embark on a transformative journey that begins with the data we rely on. Community services data is often incomplete and siloed, making it almost impossible for policymakers, decision makers and local leaders to understand the real difference these essential services are making.
Our previous analysis and reports have highlighted the potential of community services to reduce the burden on acute care, making the entire healthcare system more efficient and productive. However, to fully harness this potential, we must embark on a transformative journey that begins with the data we rely on. Community services data is often incomplete and siloed, making it almost impossible for policymakers, decision makers and local leaders to understand the real difference these essential services are making.
The status quo: community data is vast and complex
Community services cover a range of services that are delivered outside hospital, either at home or from community healthcare sites, on a same day or overnight bedded basis. They play a vital role in helping older people with complex needs remain independent at home, and often employ a highly dispersed workforce, including community nurse and rapid response teams, therapists and rehabilitation support workers.
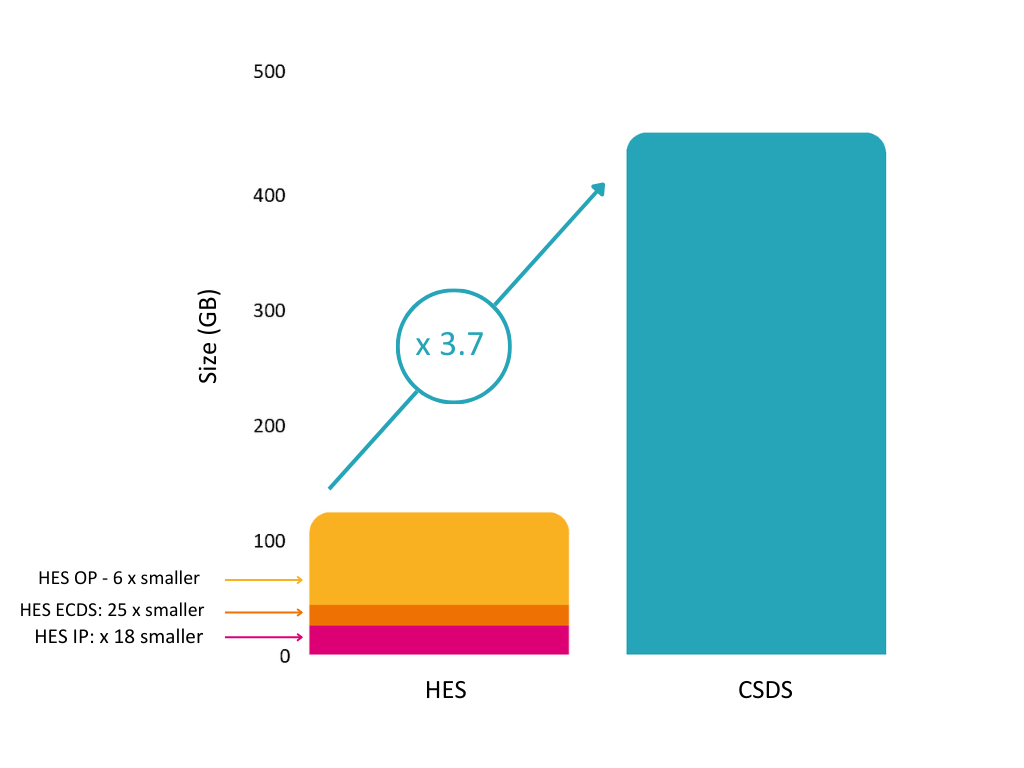
The wide range of community services available and the large number of contacts undertaken means that the Community Services Data Set (CSDS) is much larger than the acute data set (Hospital Episode Statistics, or HES).
Diagram 1: comparing the size of the CSDS to HES data sets – click to enlarge
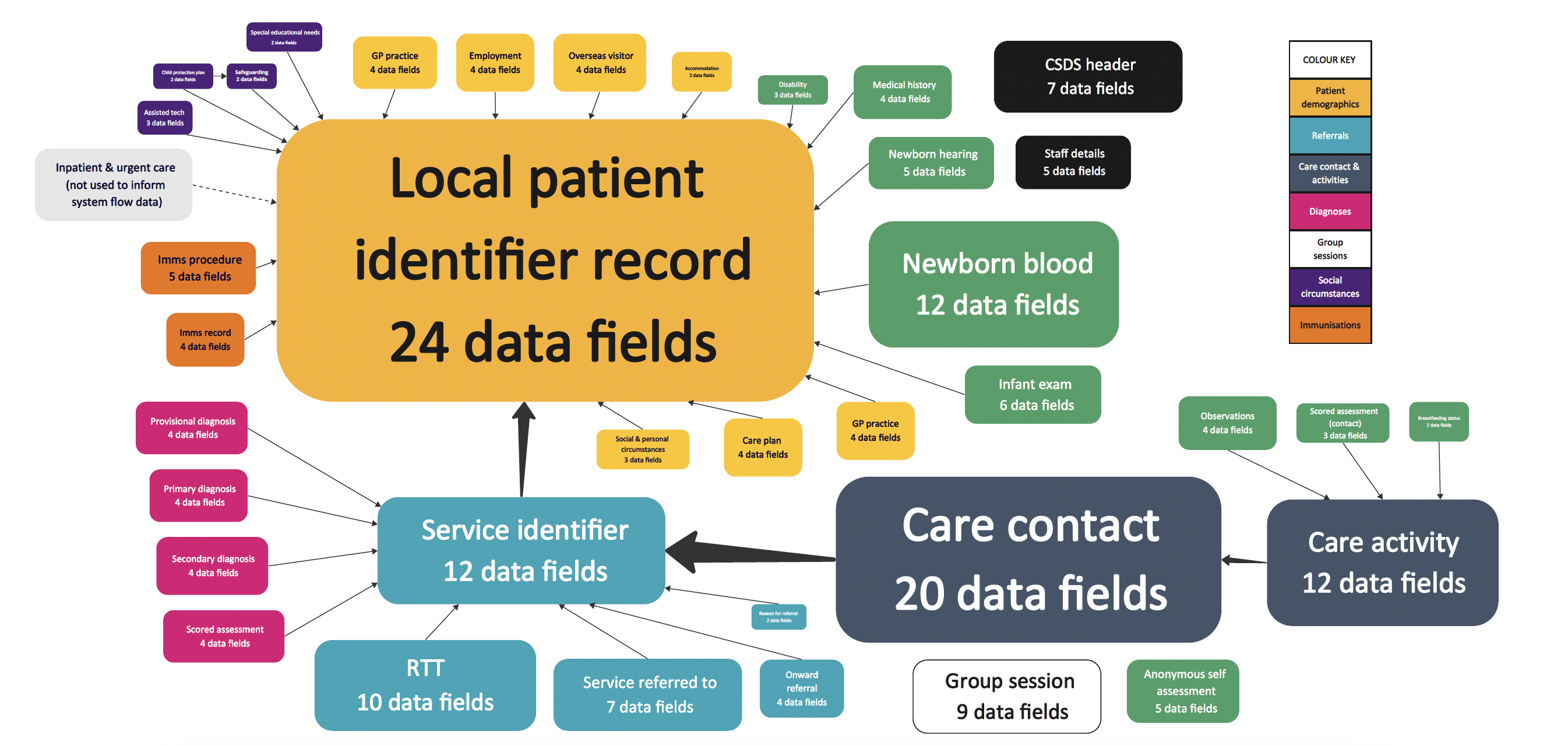
The data it attempts to capture is accordingly complex, as the following diagram shows.
Diagram 2: complexity of data within the CSDS – click to enlarge
Community data is incomplete
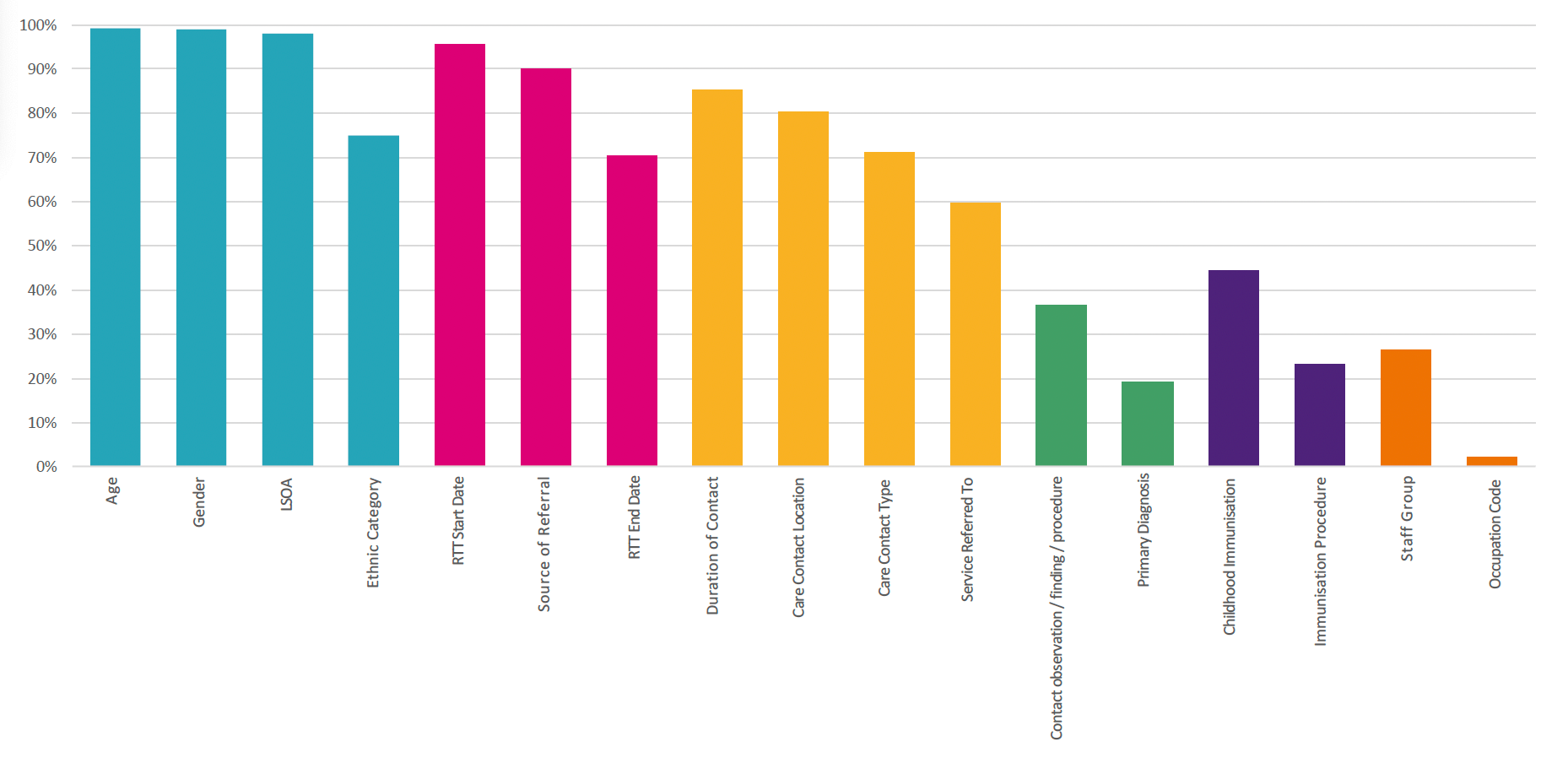
Data completeness also varies significantly across the CSDS:
Diagram 3: completeness of CSDS data fields – click to enlarge
- Most patient, referral and care type data is between 70% to 100% complete.
- Patient data is 99%+ complete, although ethnicity is only 75% complete.
- The referral start date and source are typically around 90%+ complete but drop to 70% for referral end date.
- Information about contact activity is 60 to 85% complete, with the service referred to being a critically incomplete field.
- Clinical coding data has limited completeness, with less than 40% of contacts having a clinical coding showing the observation, procedure or finding, and less than 20% of patients having a primary diagnosis.
- Immunisation is only 23% complete, although childhood immunisation is 44% complete.
- Workforce is poorly completed, with the staff group involved in treating the patient only 25% complete.
Why is the CSDS so incomplete? Alongside the large number of data requirements, providers are not incentivised to submit high quality returns in the same way that primary and acute services are, because payment is often based on a block contract rather than by results. Commissioning for Quality and Innovation (CQUIN) payments are the exception to this rule; through achieving CQUIN targets community providers can receive an increase in funding based on improvements in a number of clinical priority areas. These clinical priorities are set at the national level, by NHS England, and activity targets are agreed with providers at the local level, by commissioners.
As a result of this complexity and incompleteness, comparing community data from different ICS areas to benchmark performance is challenging– akin to comparing data apples and pears. Community data is also siloed and is rarely linked in a longitudinal dataset, linking a patient journey, so at a system level, it’s really hard to evaluate what impact community healthcare is having on local acute care – or any other healthcare, for that matter.
Analysis of completed community data shows opportunities for system efficiencies
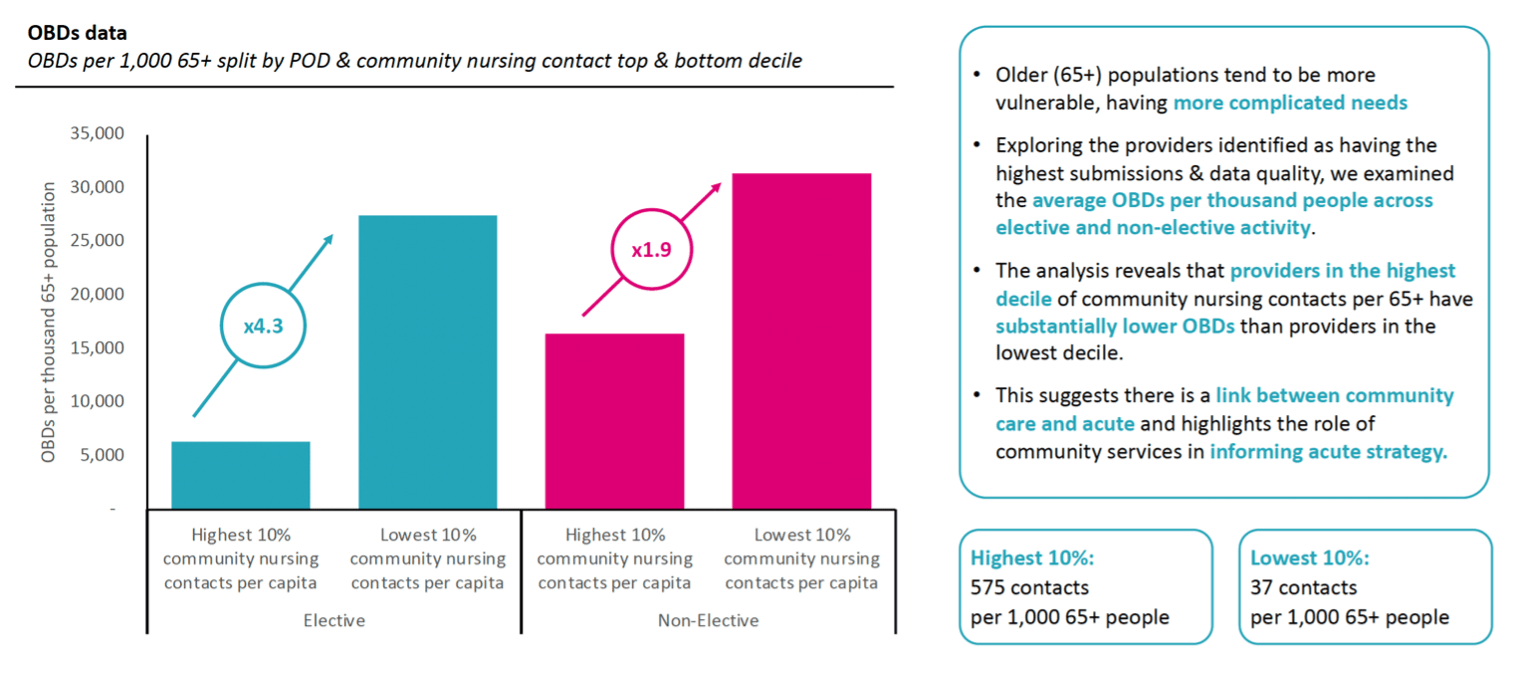
Despite these challenges, our team undertook further research into community data to determine what impact community healthcare is having on acute care. We gathered data from 32 providers representing 80% of recorded contacts in 2022. Services were reviewed to ensure that they had provided 75% of key data on their returns. The team carefully verified data with providers, before comparing it against reported acute activity in each system area.
Our research showed that areas with high community nursing contacts generally have lower amounts of occupied hospital bed days, highlighting the impact of community care on acute care. ICBs that spent a higher proportion of their expenditure on community services, generally spent a lower proportion of their expenditure on acute services.
Diagram 3: areas with high community nursing contacts have lower occupied bed days in acute care settings – click to enlarge
The analysis suggests there is a substantial opportunity to improve system productivity through investing in community care. This is especially the case given that there is a wide variation in community spend across local areas. Bringing all community spending in line with the median average spend would cost £750m, but it would also crudely save around £2.5bn in acute spend.
Improving community services through improved data – our recommendations
It’s clear that in order to effectively measure and evaluate the impact of community services investment, improved data collection and analysis is required. Our recommendations to achieve this include:
1. Prioritising the data required at a national level
Collecting vast amounts of data at the national level is not useful if this data is incomplete or inaccurate. With this in mind, there’s a pressing need to review the CSDS completion requirements, so that the most important data fields – about the patient, the healthcare activity and the diagnosis – are triaged. Until these are completed accurately, there is little point collecting other data.
2. Incentivise data completion
Improved data completion could be achieved through incentivisation, for example funding (or bonus funding) aligned to completion and submission of coded healthcare activity.
3. Standardising data collection
This includes NHS England undertaking a rapid diagnostic to understand Electronic Health Record (EHR) coverage amongst community providers, as well as the barriers they experience in completing community data returns. Following this, best practice guidelines should be produced to guide improved data collection in future, along with funding for EHR investment where needed.
4. Deploying tools for data validation
Instead of permitting the submission of incomplete data, tools could be inbuilt into data collection systems to ensure that providers have completed all required fields, and to support the verification of data accuracy.
5. Linking datasets to expand insight into what ‘good’ looks like
Once data completeness has improved, linking datasets will give further insight into the difference community services are making locally. This would be especially supported by aligning primary, community and hospital data in a longitudinal dataset, to give insight into patient journeys. This could include an ‘at a glance’ view of healthcare activity rates by age and condition, as well as all the activity in a typical clinical pathway. By leveraging in-depth workforce and finance reports, the productivity of the workforce for each community service can then be established. The return on investment of each community service, in terms of system efficiency and effectiveness, could also be evaluated.
Conclusion
Investing in community healthcare can improve NHS efficiency through a reduced need for acute care, and it can also drive economic growth. Yet, to reap these rewards fully, national and local leaders must improve the collection, accuracy and completeness of community healthcare data. Without such advancements, we remain in the dark around the true impact these services can make.
About the authors
Feargus Murphy is CF’s Head of Financial Planning and Analysis and Data Ops Lead.
Kevin Atkin is a Partner at CF.
Will Browne is an Associate Partner and leads our Data Innovation team.
Rhys Thomson is a Manager at CF.
Ben Richardson is co-founder and Managing Partner at CF, where he leads our work in Life Sciences and Data Innovation.
Read more about our team.