Unlocking the power of health beyond the hospital
Over the past 12 months, CF and NHS Confederation have published a series of reports focusing on the NHS as an investment. These involved quantifying the positive relationship between increasing NHS spending, health outcomes and economic activity, and sought to understand where additional investment in a range of settings of care could deliver the most economic output.
Most recently, we demonstrated the important role primary and community care play in creating health value and driving economic growth; we found that the UK could have seen between £10 and £14 billion additional growth if an extra £1 billion had been invested in community, primary or acute care in areas which increased spend by the least. To build on this work, we conducted further analysis on behalf of the NHS Confederation to explore how primary and community spending supports system productivity.
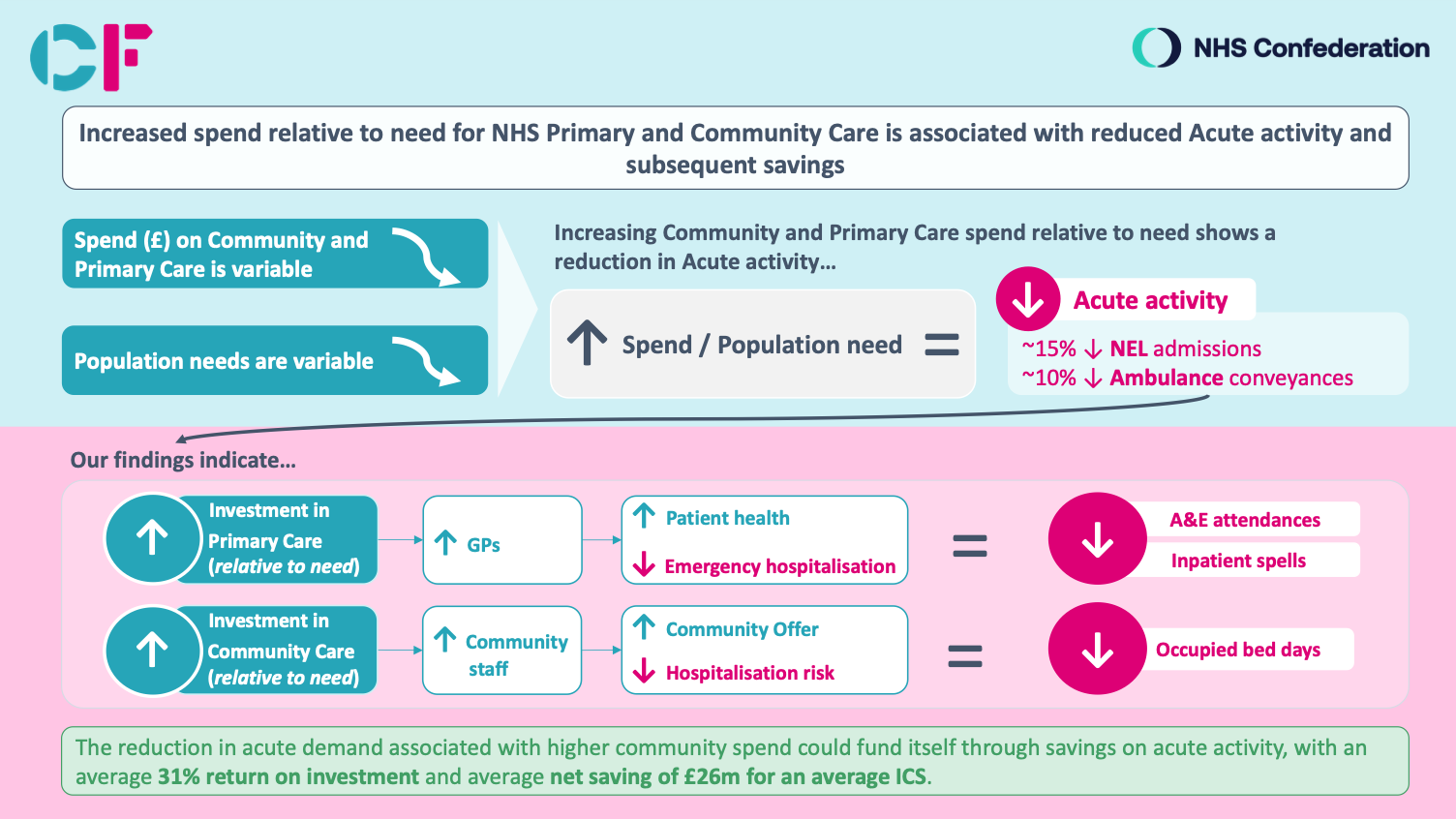
Our analysis found that:
- Those areas that spent relatively less on community care in terms of population need have seen higher-than-average levels of hospital and emergency activity, compared to those spending relatively more.
- There is no relationship between the amount invested by NHS organisations in community care and their population community care needs. Relative to other areas, some have spent more given their calculated population need while others have spent less.
- The reduction in acute demand associated with higher community spend could fund itself through savings on acute activity, with an average 31% return on investment and average net saving of £26m for an average ICS.
Findings from this analysis led us to make a series of recommendations for national government, NHS England and ICS leaders, including:
- Community spend should be prioritised as a mechanism for reducing long-term pressure on the acute sector, as a crucial contributor to healthcare system productivity and as a direct lever to provide patients with the care that they deserve.
- Providers of community health services should work with their ICSs to report operational performance and data to ensure impact is adequately understood.
- Leaders should utilise findings from this analysis to navigate challenging decisions about how to allocate resources, making significant strides in evolving toward a more preventative system that is effective both in terms of cost and care.
Our previous work in North Central London (NCL) highlighted significant inequities related to community health services that exist within a health and care system, including inequities in level of investment across geographies. A bespoke and consistent community health services offer was developed to help address some of these inequities and drive improved outcomes for residents across NCL, demonstrating a need to streamline inconsistent service offers and develop a clearer community care offer for the whole system. This is currently being implemented and includes expanding community nursing and diabetes services as part of proactive care planning.
Given this analysis, we strongly believe that community care can play a significant role in supporting system productivity and can provide ICS and NHS leaders with a direct lever of control that they can shape and use to deliver change.
Ben Richardson, managing partner at Carnall Farrar added:
“Our work shows that community services should be treated as the key to unlock system productivity and reduce pressure on the acute sector. Community care can help people who need more support to remain independent and avoid being in hospital, especially older people.
“Our research shows that areas that spend more on community care relative to need experience lower acute demand, including 15% lower non-elective admission rates and 10% lower ambulance conveyance rates.
“Additionally, we found that, despite this critical link, there is no relationship between the amount invested by NHS organisations in community care and their population community care needs. We believe this is due to the lack of a standard offer for community care and because allocation of funds to community providers is entirely at local discretion, leading to community services receiving the residual amount left after spending on everything else.
“It is through our unique access to 5 years of row-level patient data, across acute and community care, combined with publicly available national datasets and spending data that we have been able to understand the impact of investment in the community sector on system productivity.
“We strongly believe that the starting point for unlocking this potential is to prioritise, standardise, and incentivise community data collection – and using it to develop a standard offer in every ICS of what the population can expect.”
Matthew Taylor, chief executive of the NHS Confederation added:
“Acute healthcare spend has grown faster than any other area of NHS in recent years, this is simply unsustainable for the medium to long term.
“While we know we must continue to concentrate on acute spend for the time being, we also must recognise the need to ‘double run’ and then start to quickly divert where the NHS spends its budget to get the biggest bang of its buck in the longer term.
“In order to provide better care to patients and at the same time increase health service productivity more patients must be offered a higher quantity and quality of treatment in the community – either closer to, or better still, in their own homes.
“Driving a productive health service means looking across the whole system in which those services are provided, if the NHS is to survive and thrive in the latter part of this century, we need to start delivering on the long-term aspiration to shift resources into care closer to people’s homes.”
Click here to explore the research further.
Click here to read Confed’s report.
Find the Health Service Journal HSJ’s coverage of the research here