In support of developing the NHS 10-year plan, Lord Ara Darzi was asked by the Secretary of State for Health and Social Care, Wes Streeting, to envision what healthcare could look like in 2035 and chart the path to make that vision a reality.
This Future State Programme comprises four themes: a new ecosystem of health promotion and protection, faster, better and earlier diagnosis, new treatment paradigm, and innovation in healthcare delivery.
CF has been delighted to support Lord Darzi in the fourth theme of innovation in healthcare delivery. In doing so we have considered the impact that data, digital and AI can have on the NHS. We were pleased in this work to partner with Dr Devi Shetty from Narayana Health and Ravi Gurumurthy from Nesta in undertaking this research. This report set out to illustrate how data and digital technology could improve healthcare delivery in the NHS over the next 10 years.
In it we have sought to address:
- The evolution of tech trends over time
- The opportunity to transform how stakeholders interact with healthcare
- Examples of successful implementation around the world
- The implication for potential impact in the UK
- The steps required to achieve this transformation
The evolution of tech trends over time
AI has emerged as the number one theme on everyone’s lips. What’s driving it is a dramatic escalation in the performance of AI models and a simultaneous reduction in the cost. Unleashing far greater AI power at far less cost means that the application of AI will continue to leap forward, limited only by energy cost and computing power.
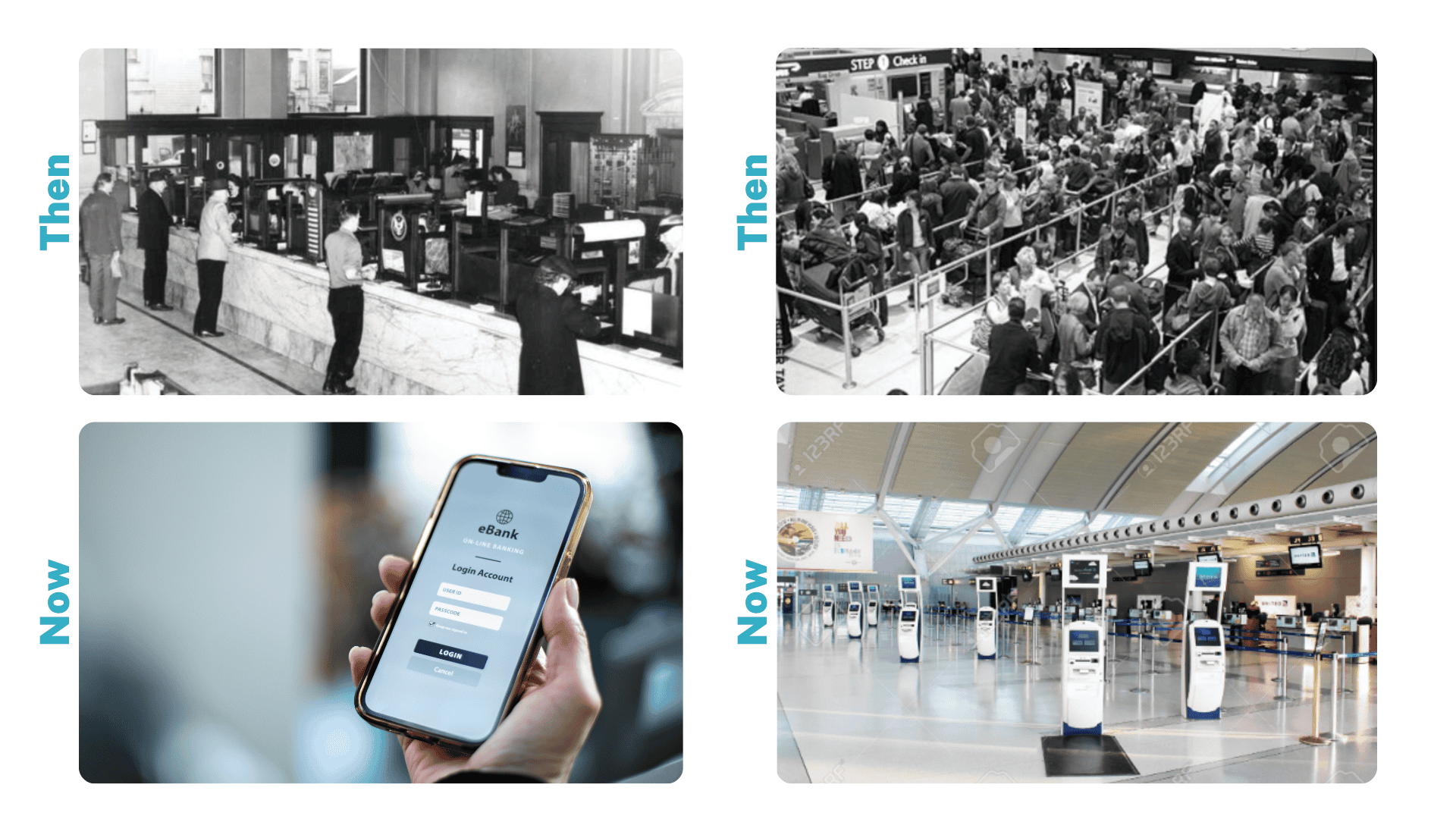
Looking at the adoption of digital technology in other industries shows healthcare has not kept pace. For example, in banking services, there’s been a shift from the use of the in-person teller and a branch to digital banking being used by almost everyone. The benefits that this brings today are convenience and efficiency, much easier control sitting in an individual’s hand, and dramatically reduced costs as banks have closed branches and largely done away with the need for tellers.
Airlines used to rely on manual process that required physical tickets and now digital apps connected to ticketing and check-in systems mean that there is an paperless experience.
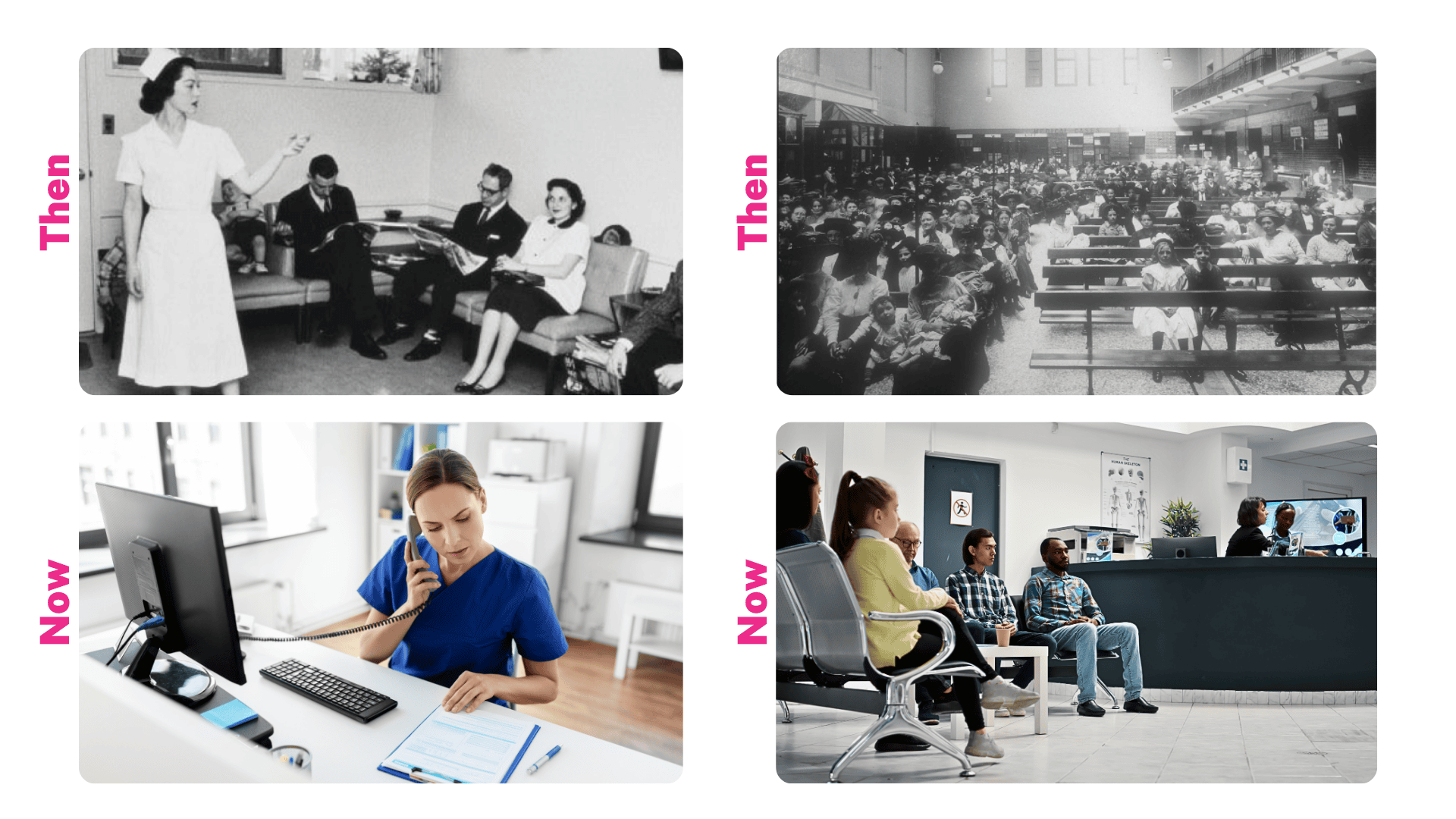
In health, access to GP services has begun to change. During the COVID-19 pandemic, we saw a greater shift to use of the telephone for interactions with the population instead of defaulting to in person. Directly messaging patients to invite them for appointments was transformative. The potential of digital appointments, particularly in digital triage and asynchronous patient review, is still developing.
Many leaders in primary care credit the adoption of technology to date as contributing to primary care productivity – i.e., being able to see more patients than ever whilst the number of GPs has declined.
In comparison, outpatient services in the NHS and around the world remain largely unchanged and clinicians widely agree that many appointments are of relatively low value. These appointments may include checking whether investigation results have been completed and ordering new ones when necessary, with multiple follow-ups sometimes required simply to verify a diagnostic result or see a patient. This process causes inconvenience for patients due to repeated travel and waiting times.
The opportunity to transform how stakeholders interact with healthcare
There is an opportunity to revolutionise how stakeholders interact within healthcare by harnessing technology to provide personalised, preventative, and proactive care. This approach empowers both patients and healthcare professionals, placing health and wellness at the forefront of our efforts.
Imagine a world where healthcare extends beyond its traditional boundaries, integrating digital advancements with the expertise of caregivers. In this transformed landscape, everyone’s health journey is unique, yet seamlessly connected to a comprehensive ecosystem of data and knowledge. Routine health screening becomes a community standard, with all diagnostic insights instantly entering digital records, that flow smoothly across borders and systems.
Gone are the days of repetitive paperwork and fragmented records. Instead, your complete health profile – from genetic predispositions to daily wellness metrics – are securely accessible as part of your health legacy, speaking a universal language that any healthcare provider worldwide can understand and build upon. This seamless integration transforms the relationship between patients and healthcare professionals, freeing them from administrative burdens to focus on what matters most: the human connection and providing better healthcare.
By leveraging technology, healthcare professionals evolve into partners in your wellness journey, their expertise enhanced by AI that processes vast amounts of health data to identify patterns and possibilities that might otherwise go unnoticed. Virtual consultations feel as natural as in-person visits, with AI assistants working in the background to capture insights and suggest personalised care pathways.
Prevention becomes the cornerstone of health, with sophisticated AI algorithms analysing patterns across populations while maintaining focus on individual needs. In this world, wearable devices transcend simple step tracking, becoming part of an intelligent network that anticipates health challenges before they arise. Agents may provide nudges to you to support healthy habits and preventative health interventions. Digital therapeutics adapt in real-time to your needs, offering personalised support for everything from chronic condition management to mental wellness, available whenever and wherever you need them.
Planning for future healthcare needs becomes more precise and proactive, with all stakeholders working from the same rich pool of insights. Healthcare leaders are empowered to design services that meet people’s needs while freeing staff from administrative burdens. The result is a healthcare system that not only treats illness but nurtures wellness, enriching life through the seamless integration of digital innovation and human compassion, creating a healthier, more connected world, where living well becomes a daily reality.
There’s clearly huge potential to leverage the power of technology to deliver personalised, preventive and proactive care that empowers patients, the workforce and puts health and wellness at its core. Data, digital and AI should change the experience for patients, care providers and regulators.
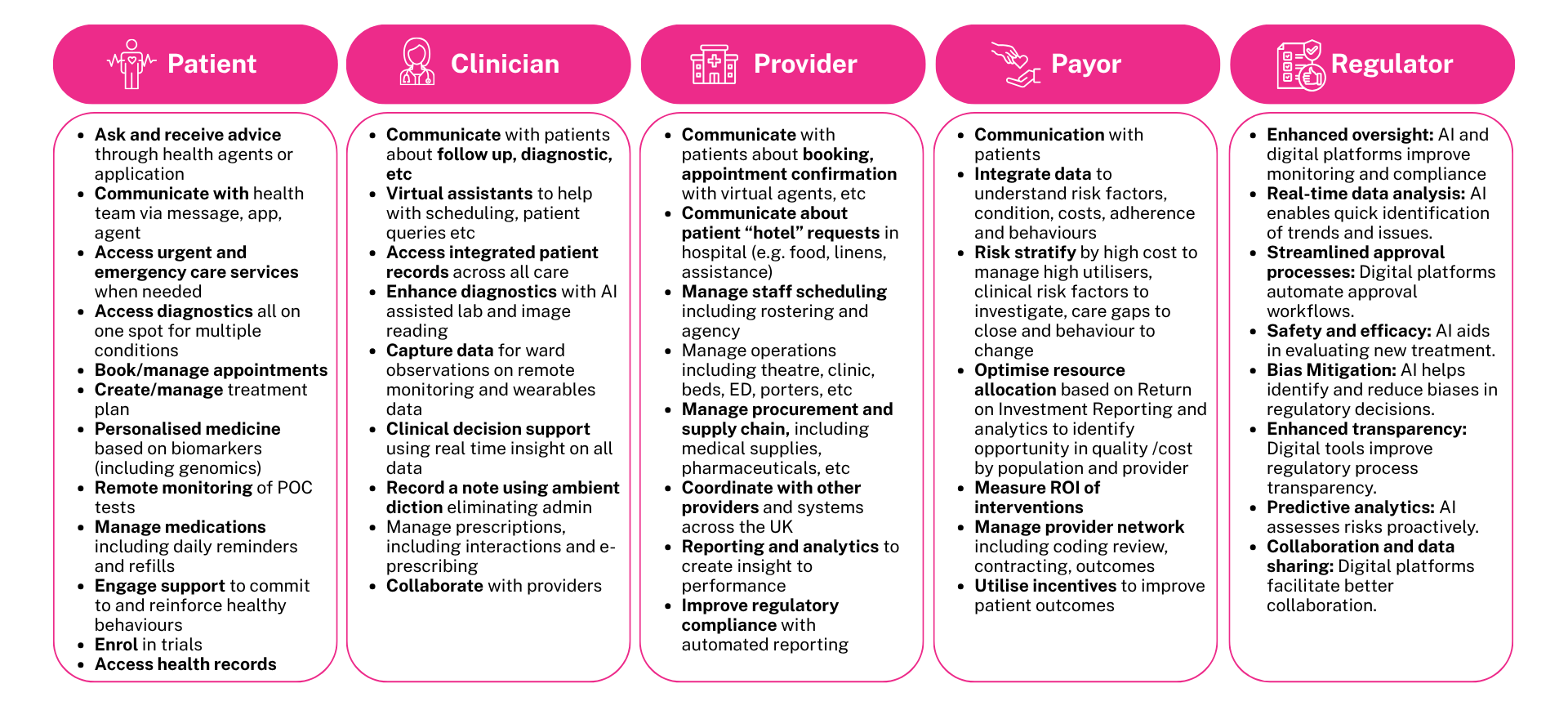
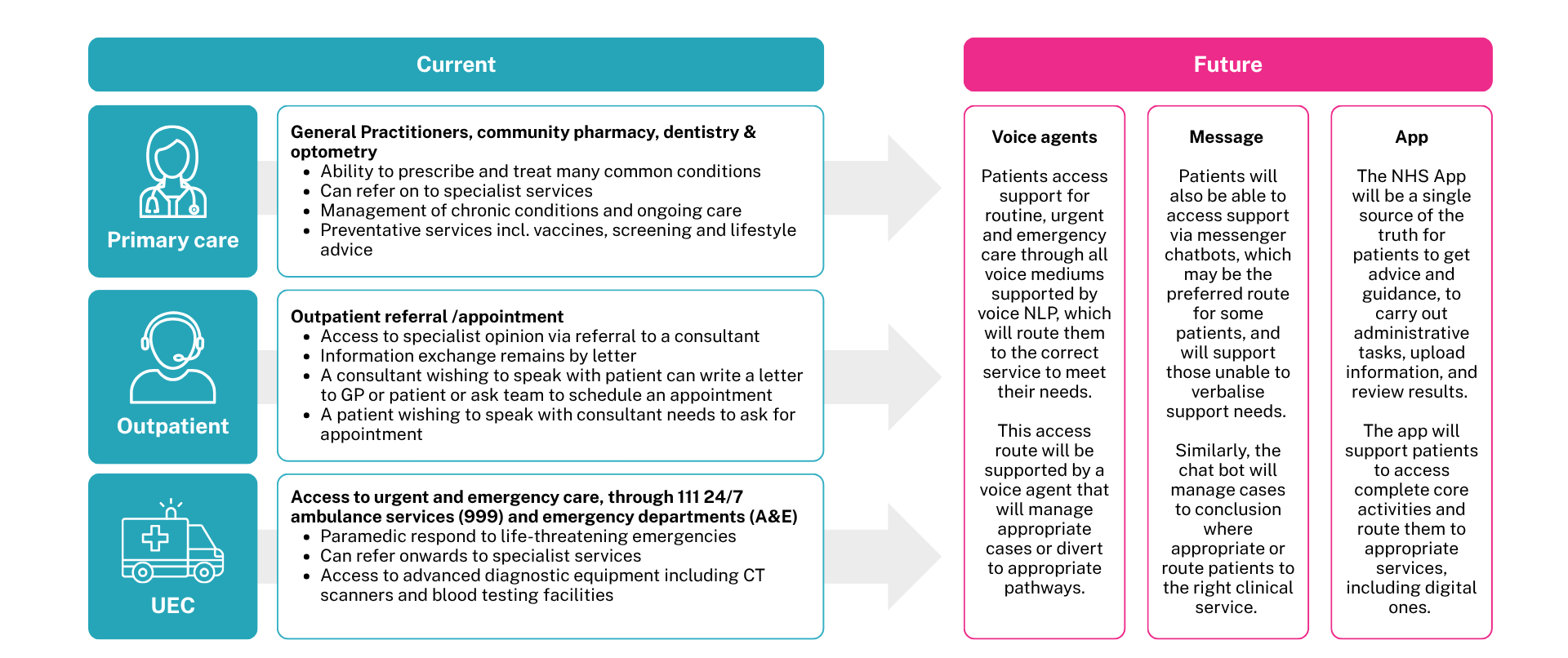
Currently, individuals access health services through three main channels: primary care, outpatient services, and urgent or emergency care via ambulance or Accident & Emergency (A&E) departments. In future, the primary entry point to health services should be digital-first, enabling interactions through voice agents, messages, and applications. Even where someone is picked up by ambulance there should be digital communication between the ambulance and A&E that helps to manage this flow. This approach has the potential to streamline communications across all services, providing greater convenience and efficiency.
To try to illustrate this, we can consider what the patient’s journey through outpatient care will look like and how it can significantly accelerate the patient pathway.
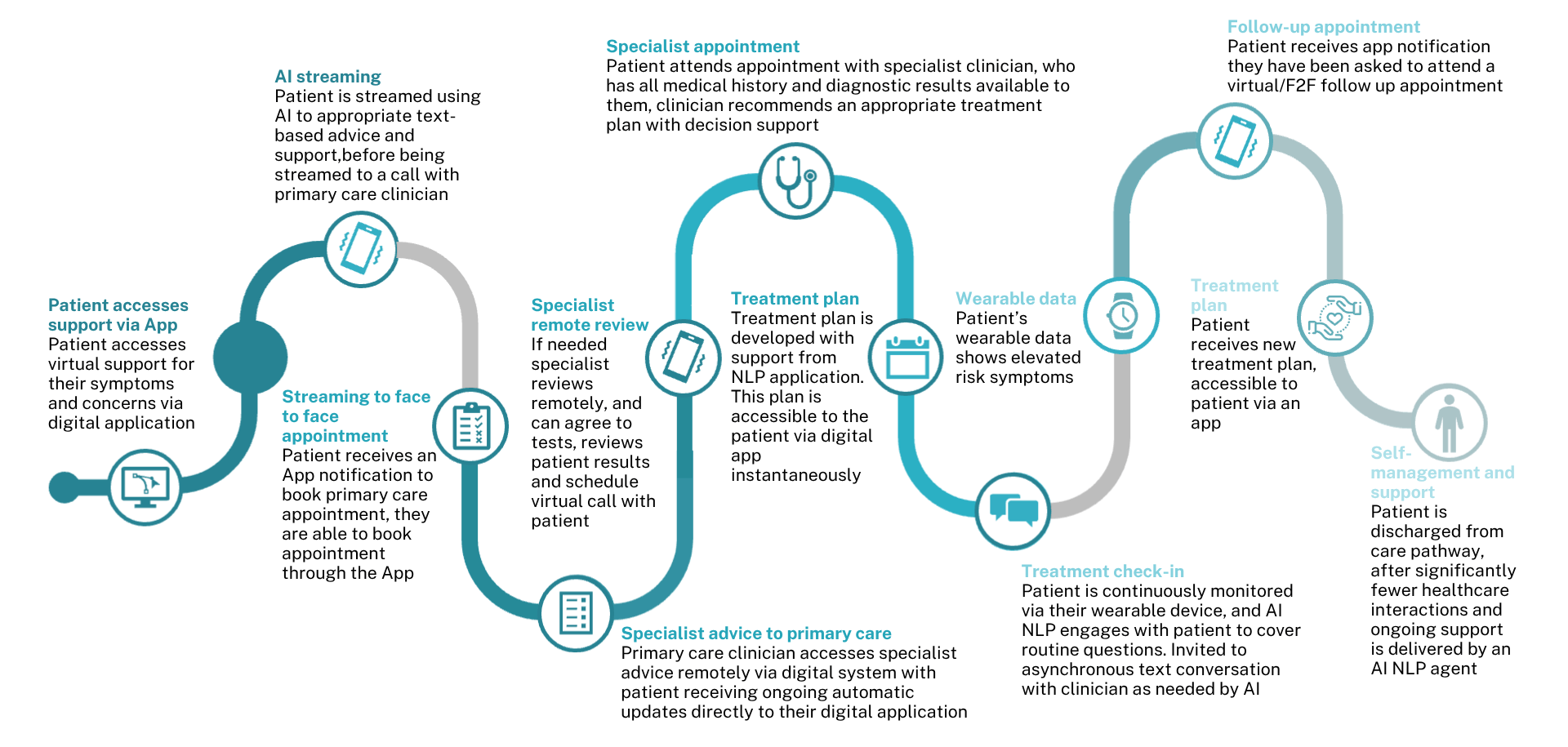
Similarly, this approach can be conceptualised and illustrated across a variety of different contexts for example in new diagnosis of a chronic condition, within a patient’s elective inpatient journey through to their journey from an Intensive Care Unit (ICU) and discharge.
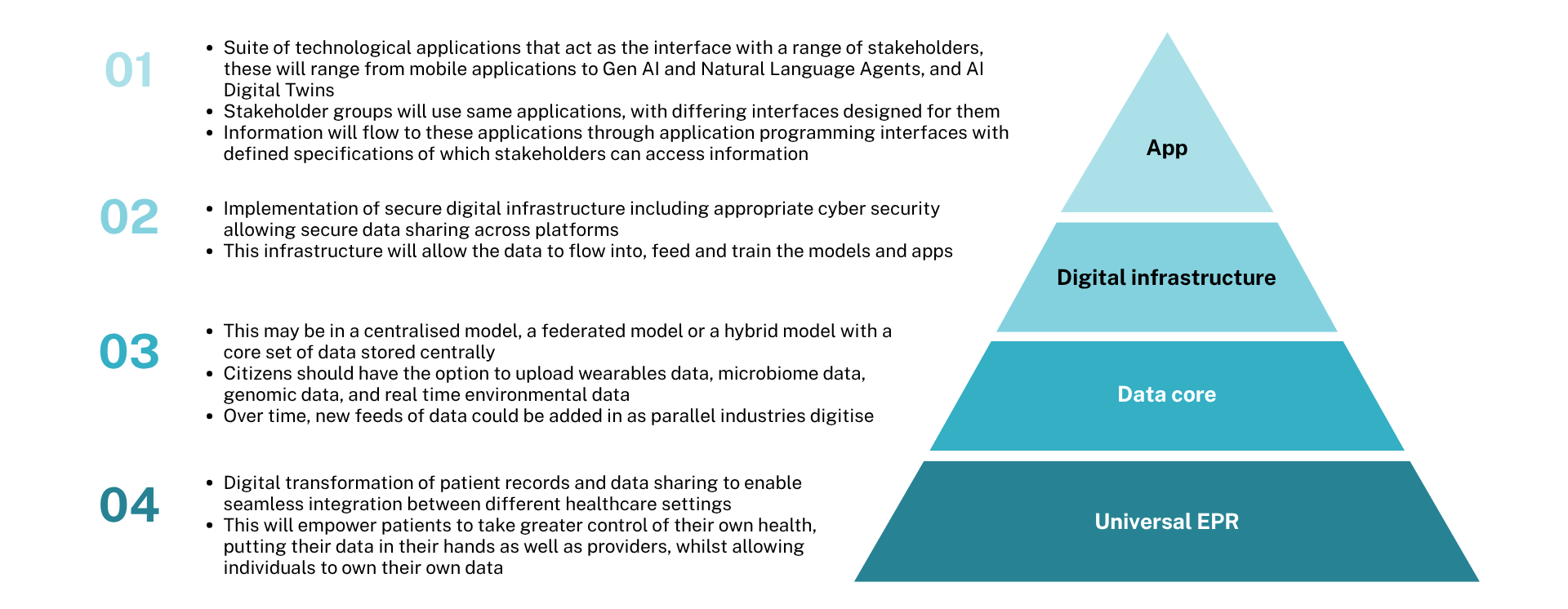
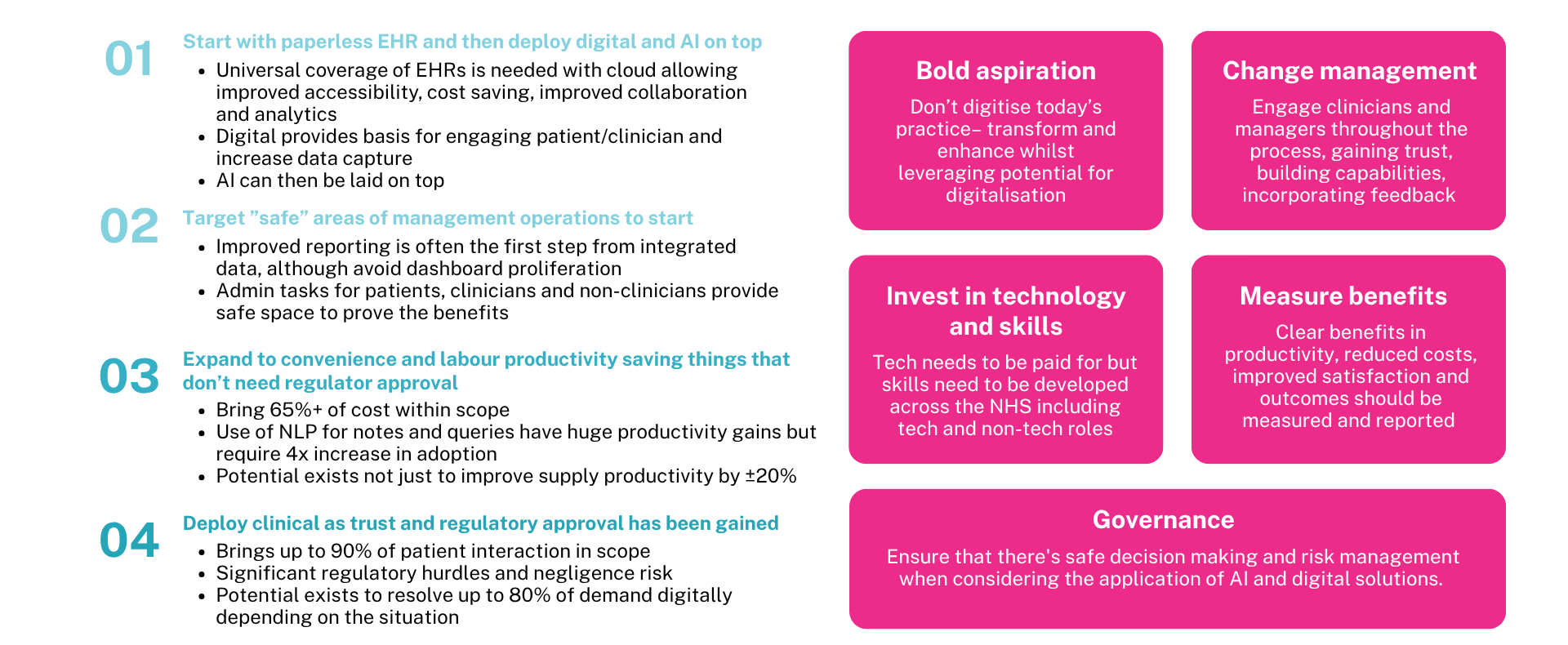
To achieve this goal, health systems and providers must start with a foundation of universal data that forms the digital basis for user-centric care. This requires the implementation of a universal electronic EPR (Electronic Patient Record) with an integrated data core. From this foundation, they can establish the digital infrastructure necessary for seamless interaction and apply AI-driven applications to engage stakeholders. A commonly observed progression involves transitioning to paperless EPR systems as the initial step, followed by enhancing systems with integrated data, digital tools, and AI capabilities.
Examples of successful implementation around the world
This report examined successful cases globally that have promoted the adoption of integrated data, digital, and AI technologies. Individual places around the world show that significant progress is already being made. And, in some places, the transformation of entire providers or health systems can be seen. While this vision may seem distant for some, including the NHS, it is already a reality today in parts of India.
Narayana Health is one of the largest multi-specialty hospitals in India with 7000 beds, 23 hospitals across 47 facilities with 20,000 staff creating a centre of excellence, especially in cardiac surgery that delivers up to 15% of the total cardiac care cases across all of India.
Its rapid growth meant that it had many manual and Excel-based processes that were unsustainable. The existing performance and analytics capabilities were inadequate to support organisational growth, leading to a rapidly increasing workforce and an unsustainable cost structure. This issue was particularly significant because 80% of Narayana’s patients are self-paying and typically have low incomes.
Narayana has embarked on a journey focused on implementing a Universal Digital EPR system, complemented by tools to support administrative functions and operations. The organisation established core metrics to measure revenue growth, operational costs, and workforce productivity. They developed proprietary in-house solutions, featuring a robust data platform along with a universal EPR and applications designed for both patient and clinician use. Additionally, they restructured their clinical and non-clinical processes to incorporate a digital-first approach.
It now has a complete view of the patient pathway and collect turnaround data for every station in every hospital to identify and resolve bottlenecks and respond to emerging patient flow challenges. They invested in proactive comprehensive diagnostic health checks at scale to enable earlier intervention and significant cost reductions. They also created one of the world’s largest telemedicine networks, increasing their reach without requiring additional physical estates, using mobile outreach vans and semi-urban diagnostic centres.
Key drivers of operational efficiency include real-time wait time monitoring, advanced analytics, AI-driven bookings, improved resource planning, AI to reduce turnaround time, and digital document assistance using natural language processing and voice-activated tools. Additional factors include AI for scanning, tagging clinician-relevant documents, and supporting diagnostics.
The result has been significant growth at a lower cost. It is estimated that care provided by Narayana is 40% less expensive than that of their competitors, which offers a competitive advantage in the market, as 80% of their patients are self-paying and come from generally low-income backgrounds. There are also stunning examples of impact across ambulatory care and nursing.
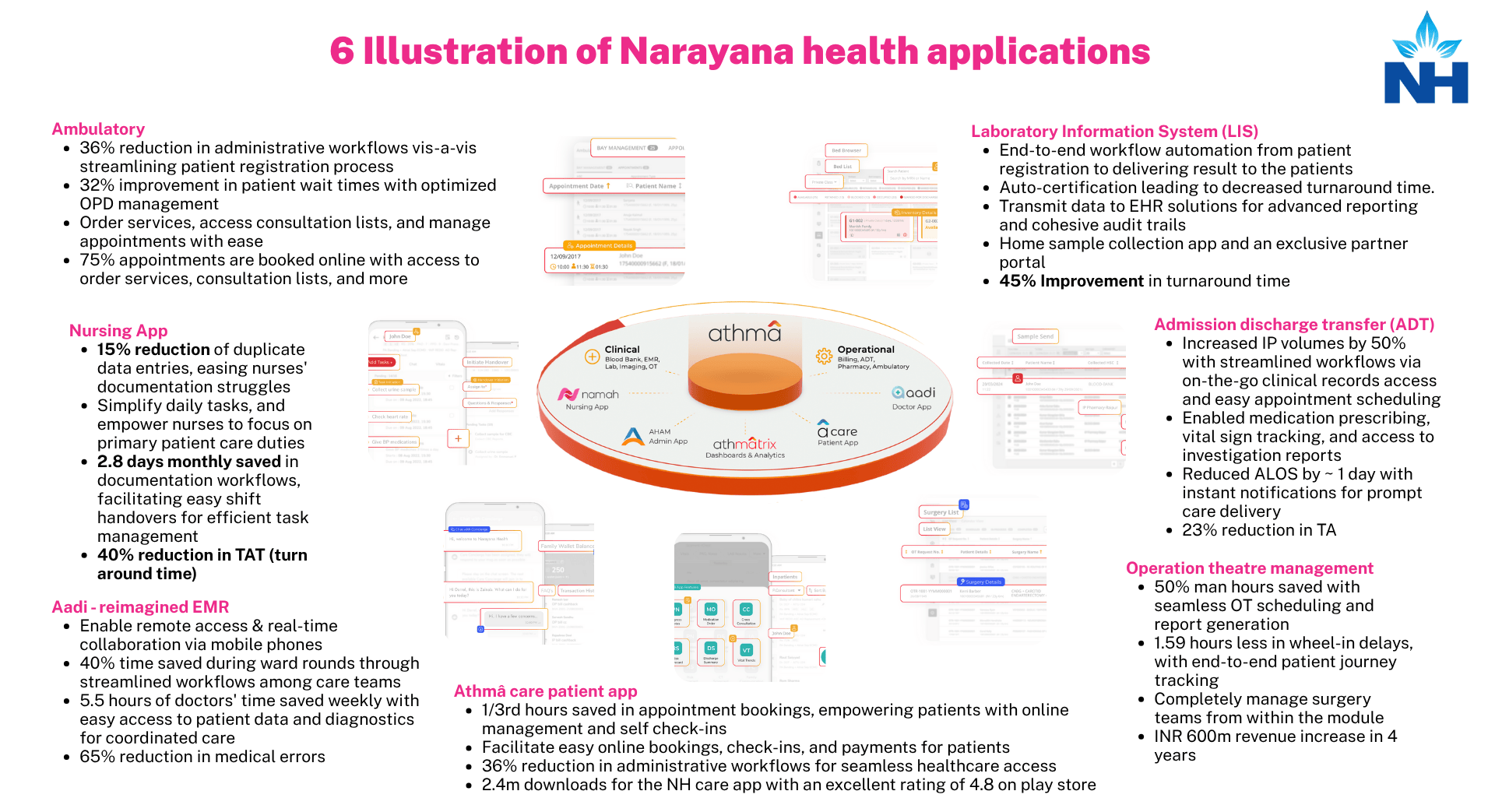
In ambulatory care, there’s been a 36% reduction in the administrative workflow that is needed, with 75% of patients booked online with access to order services, consultation lists and more. A nursing app has resulted in 2.8 days per month saved from each nurse in the documentation of workflows. The EMR has enabled the collection of patient observations with a 40% time saving in ward rounds because of the workflows being optimised, which means there’s 5.5 hours of doctor’s time per week saved due to easy access to patient data.
Their lab system is able to run automated end-to-end workflows. Their admission, discharge and transfer has increased patient volumes by 50% on the same bed base because of streamlining the workflows and reduced length of stay by a day with instant notification for advancing the workflow towards discharge and a 23% reduction in turnaround time. In theatres, there’s been a 50% reduction in the man hours needed for staffing with 1.6 hours less delays per day in the end-to-end patient journey and an increase in revenues.
The Athma Patient Care app resulted in a third of administrative time being saved because appointment bookings are done automatically, enabling patients to interact in natural language voice to book an appointment in a convenient, conversational way, instead of being stuck in a voicemail tree.
If such an impact is achievable in India, despite its resource constraints, it should be possible to accomplish it more swiftly in developed nations. We have also highlighted examples from various global companies and systems that have endeavoured to enhance workforce productivity, improve clinical outcomes, and achieve overall system improvement.
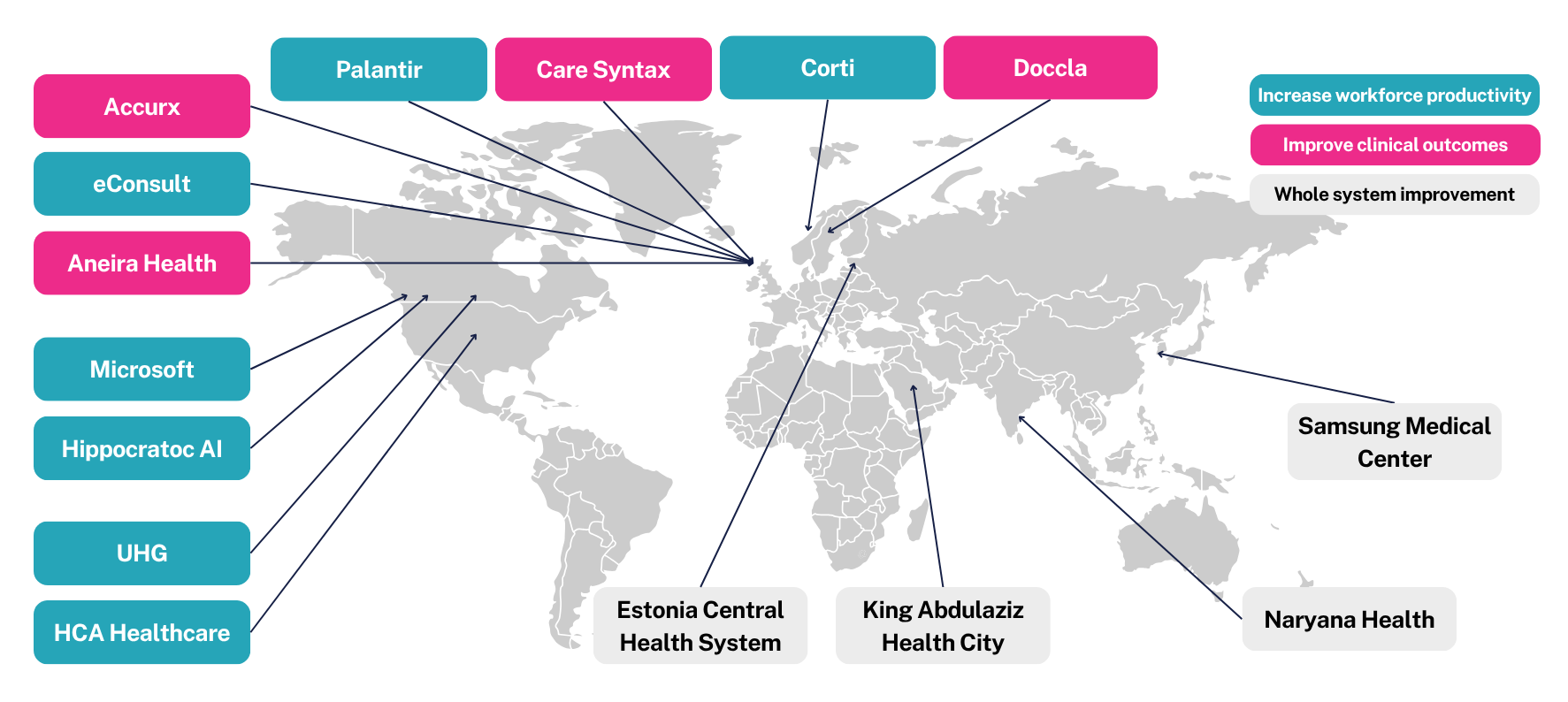
Initially, these technologies are applied to non-clinical areas of management and operations – domains that are considered safe, as they are neither clinically sensitive nor subject to the same regulatory oversight. The next phase targets areas focused on convenience and labour productivity, which similarly avoid regulatory hurdles but deliver significant value by capturing efficiency gains.
Only after establishing a strong foundation and demonstrating tangible benefits do these initiatives expand into clinical domains – once trust is established and the necessary regulatory approvals are in place.
The last point is about establishing the governance, to ensure that there’s safe decision making and risk management when considering the application of AI and digital solutions. The NHS is well used to the notion of cybersecurity for digital solutions, but the application of AI on top raises questions about decision making and whether something needs to have a medical device classification.
The application of AI itself raises questions about whether it serves as a decision prompt or a decision maker. It is important to determine the role of humans in this process and establish an appropriate framework. Additionally, organisations need to implement governance and controls to ensure clinical decisions and patient interactions utilise AI securely and appropriately, while ensuring that AI models adhere to established standards.
The implication for potential impact in the UK
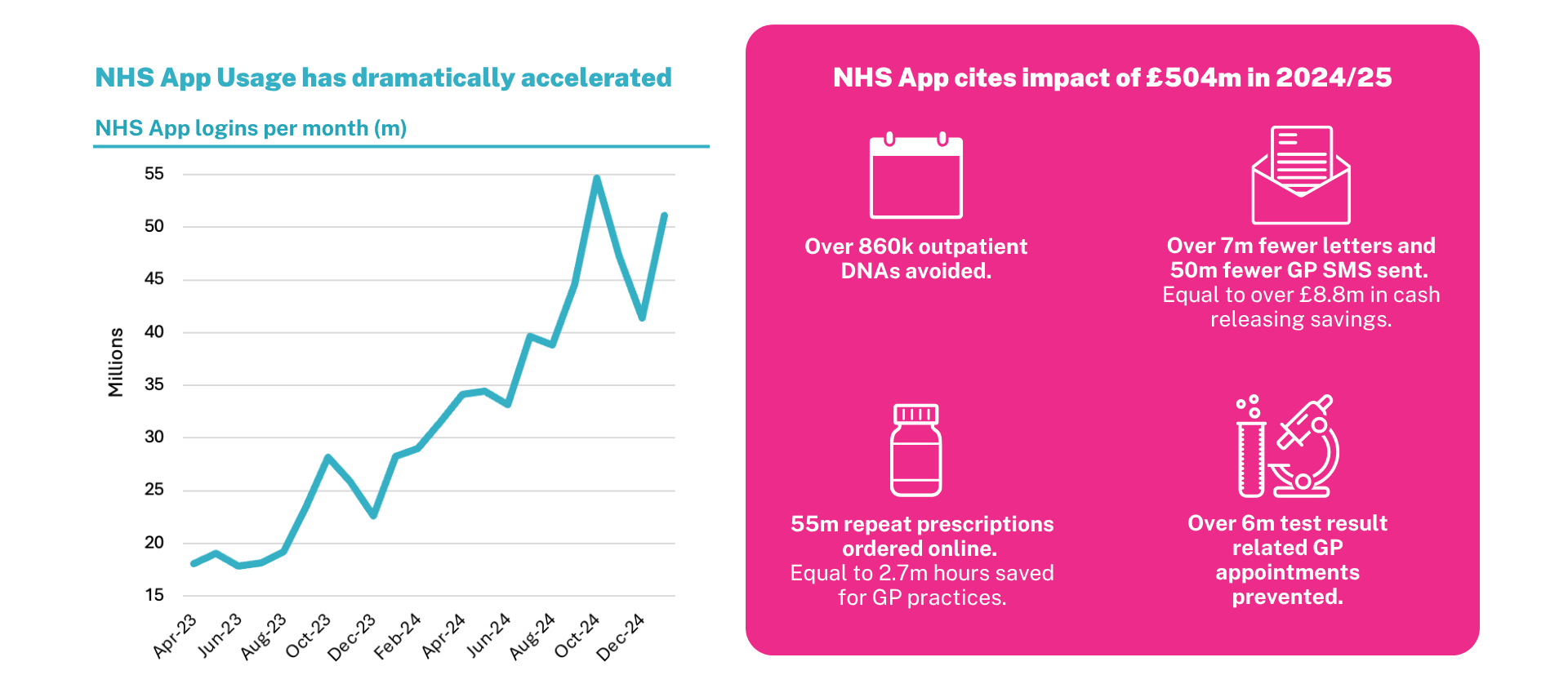
Looking at how the NHS is pursuing data, digital and AI, three key planks are the use of the Federated Data Platform, which represents a £330 million investment, the NHS App, which emerged during the pandemic as a key interface and has been seeing steadily increasing engagement with the population, and the adoption of Microsoft Copilot and other large language models that have been trialled and piloted across the NHS.
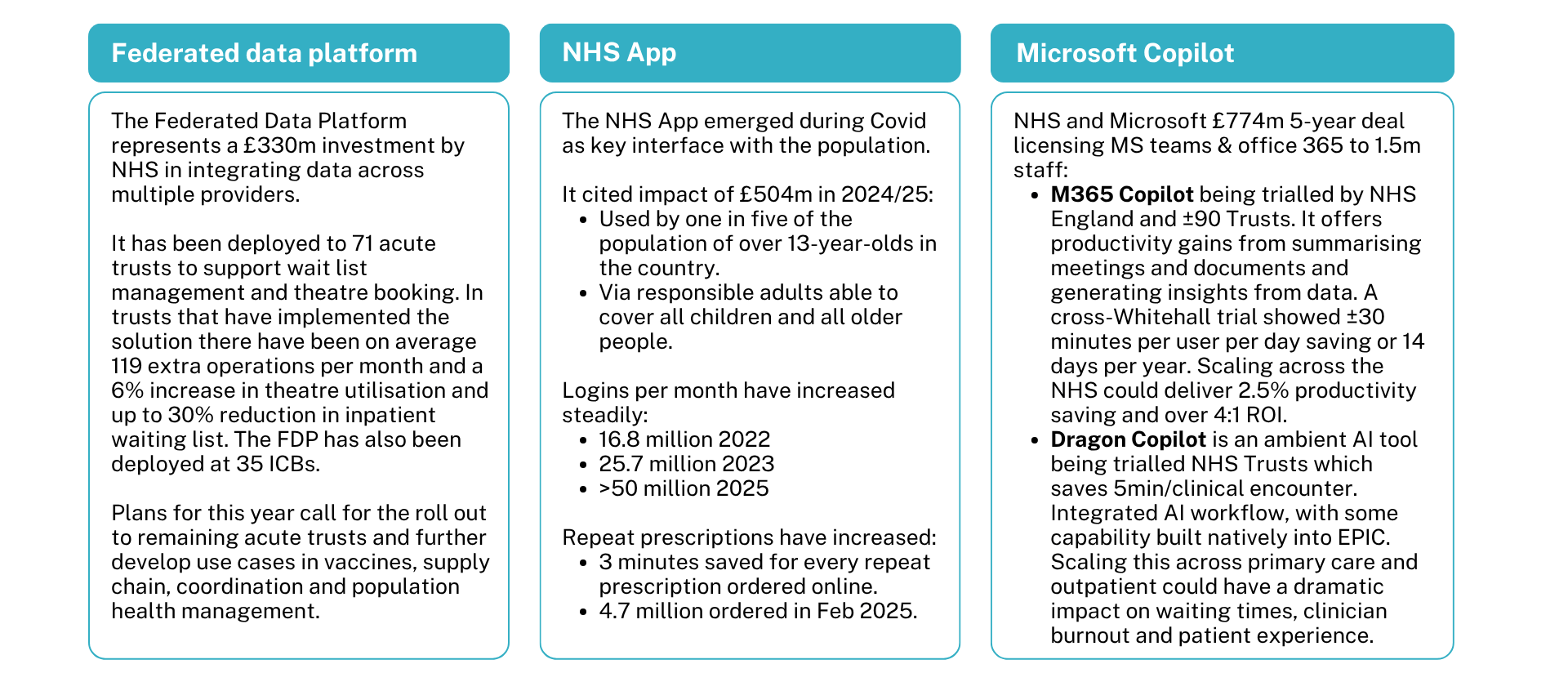
The NHS App has illustrated the tremendous power of engaging the entire population through a digital front door. Consumer enthusiasm for data, digital and AI has already begun to be shown – and has already started to generate significant savings.
The digital and AI opportunity to bend the cost curve
What we can expect to be able to see from this is improved clinical outcomes by being able to identify opportunities earlier. The backdrop is the steadily rising healthcare costs that have tended to grow 1.5% faster than GDP on a per capita basis. And the critical question is whether data, digital and AI can help to bend that cost curve.
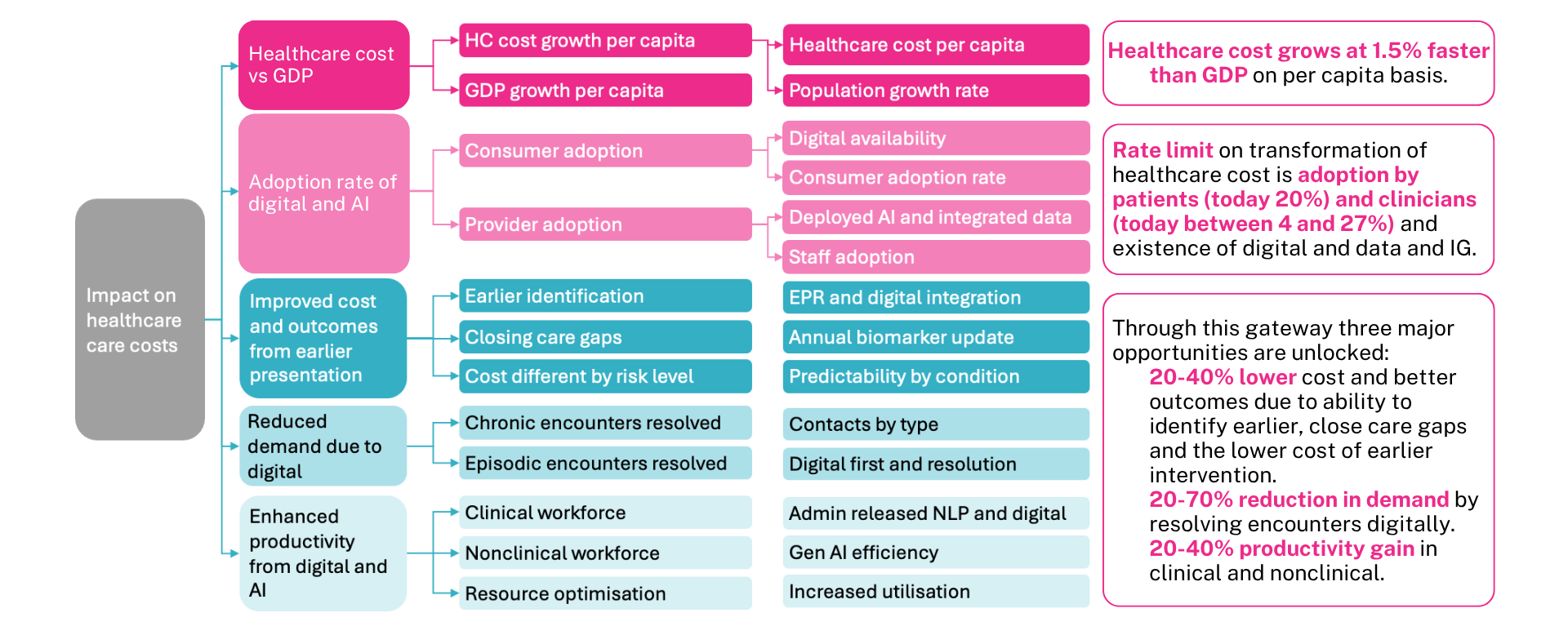
Looking at the opportunities of improving cost and outcomes from earlier intervention, reducing demand by resolving it digitally, and enhancing productivity, we have estimated individual points could each save between 20 and 40% in reduced costs or 20 to 70% reduction in resolution of demand or 20 to 40% productivity gain. If you multiplied all those together, it could potentially cut costs in half. However, the rate limiting step of this is the adoption by patients, by clinicians, and by organisations. This will be the result of both the individual decisions that patients and clinicians make and the organisational decisions and commitments that are made to adopt AI.
CF has examined the possibility of addressing demand through digital means. By using a panel of clinicians and analysing data, interviews, and case examples, the potential for both initial engagement and digital resolution has been identified. The ability to predict disease, including chronic diseases and cancer, is achieving accuracy rates of 80-95%.
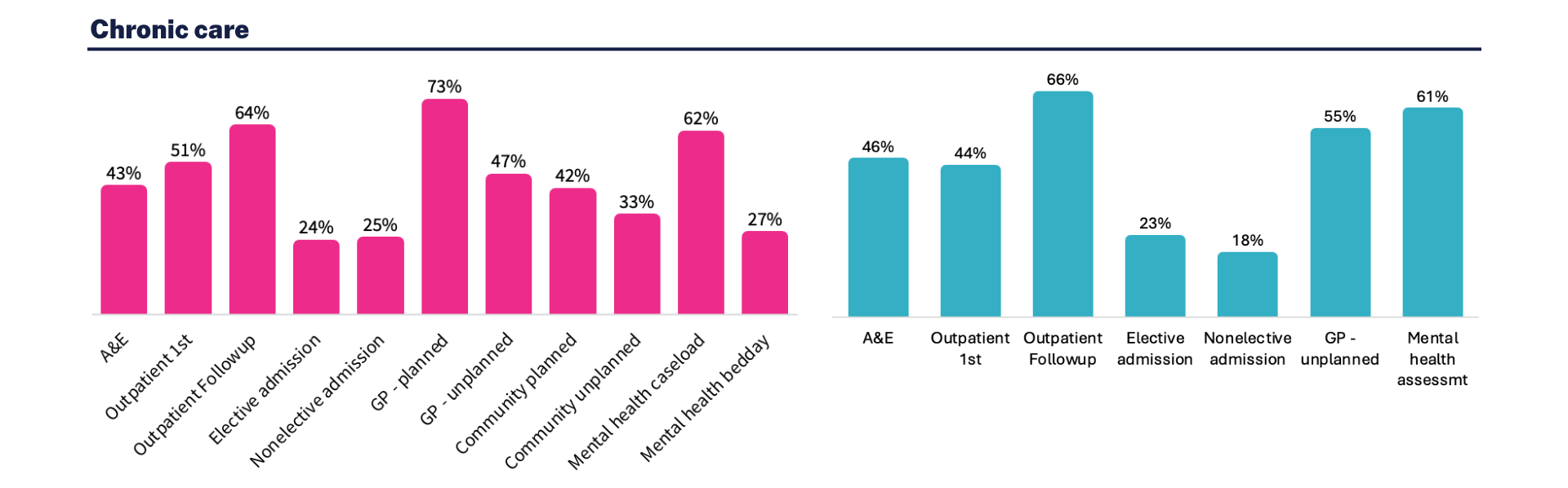
Interviews and case studies indicate asynchronous digital engagement via App, message or voice presents the opportunity to reduce demand particularly in chronic care:
- First engagement: capture information including presenting condition, relevant history, diagnostics, accessing integrated data, and leveraging AI tools to ensure routed appropriately.
- Digital resolution: resolving patient’s complaint through digital channels, used to advise on course of action and/or manage submission of remote monitoring, capture of routine follow up information, providing advice.
A CF clinician research panel assessed the potential impact of data digital and AI across different settings of care:
- 43-66% of ambulatory hospital contacts
- 18-25% of hospital admissions
- 47-73% of primary care contacts
- 61% of ambulatory mental health contacts.
One of the most exciting areas is the steadily increasing predictive accuracy of algorithms to help identify major health conditions, whether it’s cardiovascular, diabetes, chronic kidney disease, dementia or cancer. As these accuracy rates steadily increase, the potential to intervene earlier and change the course of disease is dramatic. For instance, 45% of dementia cases may be preventable, and there’s a dramatic reduction in mortality and costs by catching cancer at stage 1 instead of at stage 4.
The second domain is the ability to resolve demand digitally. The third area is the tremendous power of natural language processing and GenAI to offer substantial savings in clinical and non-clinical time that create productivity gains. There have been multiple examples cited of the ability to save time from clinical documentation, estimating to be in the range of 13 hours per week, or five minutes per encounter by others, or being able to achieve faster results when searching for information, increasing the efficiency of knowledge workers by between 30 and 60 minutes.
The steps required to achieve this transformation
Enabling this vision needs seven key things in place: integrated data and digital transformation, driving the adoption of applications, seeing the adoption of AI, regulatory policy around AI, commissioning of digital solutions, skills and capabilities, and governance in place to be able to implement these changes safely and effectively.
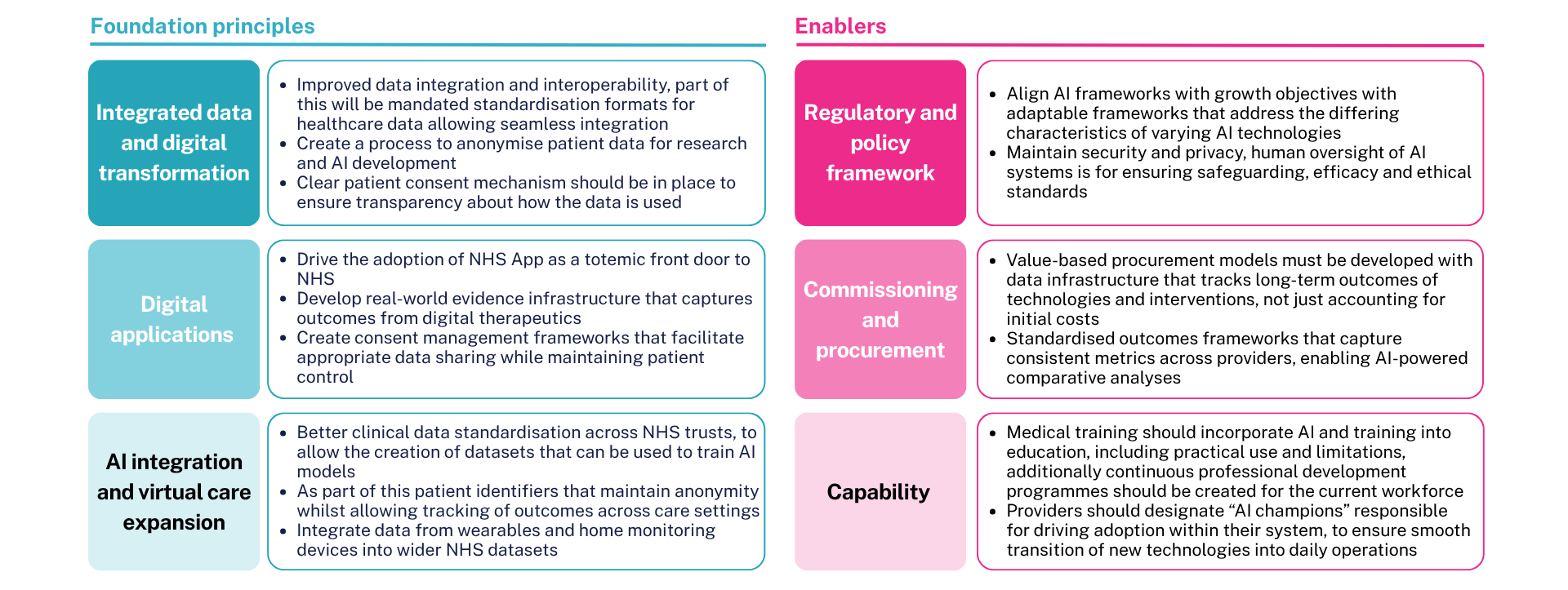
Experience with various healthcare systems indicates that effective transformation relies on committed leadership rather than perfect conditions. The NHS has notable strengths in population health data and integrated care models and can learn from organisations like Narayana Health. However, each system must develop its own transformation strategy based on its specific strengths, constraints, and opportunities.
As transformation advisors, we’re seeing a clear divide emerging between healthcare organisations that are preparing for the future and those that are still fighting to preserve the past. The organisations in the first category are investing in comprehensive digital capabilities, redesigning their operating models, and preparing their workforces for AI-augmented care delivery.
The digital future of healthcare is not a distant prospect; it is currently being implemented by leading organisations globally. The question isn’t whether transformation will happen, but whether organisations like the NHS will lead it or be disrupted by it.
About CF
CF is a leading consultancy dedicated to making an enduring impact on health and healthcare. We work with leaders and frontline teams to improve health, transform healthcare, embed life science innovation and boost growth through investment. With unmatched access to UK healthcare data and award-winning data science expertise, our team are a driving force for delivering positive and meaningful change.
About the authors

Ben Richardson
Ben Richardson is a Managing Partner at CF, leading Life Sciences and Data Innovation. With two decades of experience, he has worked with health systems and life sciences companies globally, focusing on strategy, transformation, and development. Ben has contributed to primary care, diabetes, cardiovascular, cancer, mental health, and population health management. Since 2014, he has helped CF become an award-winning healthcare company in management consulting and data services.

Dr Zahra Safarfashandi
Dr Zahra is a partner at CF, and Chief Executive of CF GCC, our Middle East entity. She is a clinician and an experienced healthcare management consultant. She specialises in implementing clinical and digital transformation programmes at scale. She has worked across the UK, Europe and the Middle East focused on improving clinical outcomes, workforce productivity and operational effectiveness by leveraging clinical best practice and digital innovations.

Yemi Oviosu
Yemi is a Senior Manager at CF with a PhD in Cardiovascular Biochemistry, specialising in strategy and scaling innovation for healthcare and life sciences clients. He focuses on evaluating and implementing digital technologies that enable population health management and driving sustainable, enterprise-wide transformation. His unique blend of scientific insight and technology-strategy expertise helps clients accelerate innovation, de-risk investments, and improve patient outcomes.
With special thanks to Elise Kearsey, Beena Mistry, Colette Russell, Lali Sindi and Gauri Patel.