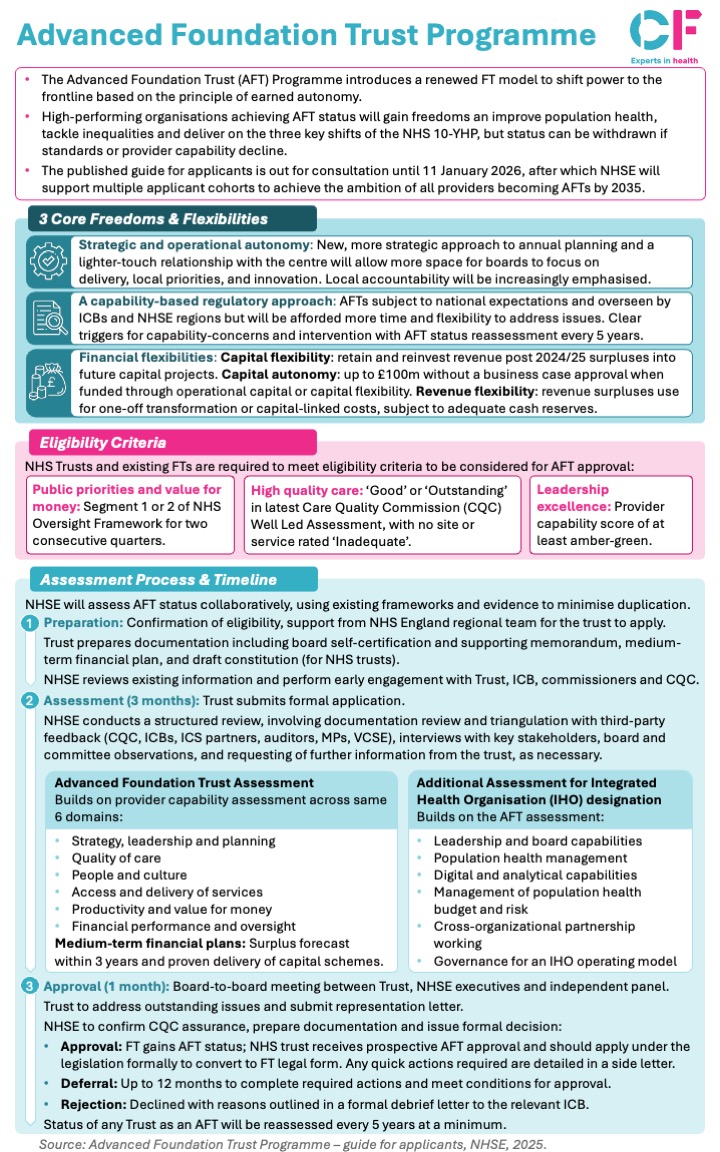
NHS England has published its guide for applicants to the Advanced Foundation Trust (AFT) Programme, introducing a renewed foundation trust model designed to shift power to the frontline based on the principle of earned autonomy. The programme represents a significant evolution in how high-performing NHS trusts will be recognised and empowered, directly supporting the three key shifts outlined in the NHS 10 Year Health Plan: sickness to prevention, hospital to community, and analogue to digital.
High-performing organisations achieving AFT status will gain new freedoms to improve population health, tackle inequalities and deliver on these strategic priorities. However, the guide is clear that status can be withdrawn if standards or provider capability decline, maintaining accountability alongside increased autonomy.
The published guide is currently out for consultation until 11 January 2026, after which NHSE will support multiple applicant cohorts to achieve the ambition of all providers becoming AFTs by 2035.
Key headlines
Strategic and operational autonomy
AFTs will adopt a new, more strategic approach to annual planning with a lighter-touch relationship with the centre, allowing more space for boards to focus on delivery, local priorities, and innovation. Local accountability will be increasingly emphasised alongside this increased autonomy.
A capability-based regulatory approach
AFTs remain subject to national expectations and oversight by ICBs and NHSE regions but will be afforded more time and flexibility to address issues. The programme includes clear triggers for capability concerns, with AFT status reassessment taking place every 5 years to ensure standards are maintained.
Financial flexibilities
The programme introduces three types of financial flexibility:
- Capital flexibility: AFTs can retain and reinvest revenue post 2024/25 surpluses into future capital projects
- Capital autonomy: Access to up to £100m without a business case approval when funded through operational capital or capital flexibility
- Revenue flexibility: Revenue surpluses can be used for one-off transformation or capital-linked costs, subject to adequate cash reserves
Eligibility criteria and assessment process
To be considered for AFT approval, trusts must meet three core criteria: Segment 1 or 2 of NHS Oversight Framework for two consecutive quarters, ‘Good’ or ‘Outstanding’ CQC Well Led Assessment with no ‘Inadequate’ ratings, and provider capability score of at least amber-green. The 4-month assessment process includes preparation (eligibility confirmation and documentation), assessment (3 months of structured review with third-party feedback from CQC, ICBs and stakeholders), and approval (1-month board-to-board meeting leading to approval, deferral up to 12 months, or rejection).
The assessment builds on provider capability across six domains including strategy, quality of care, financial performance and medium-term financial plans, with additional assessment for IHO designation covering population health management and digital capabilities. AFT status will be reassessed every 5 years.
Download our snapshot below for a full summary:
Why does it matter?
The AFT Programme represents a significant shift in NHS governance, moving from centralised control to earned autonomy based on demonstrable capability and performance. For high-performing trusts, AFT status offers the freedom to innovate, invest strategically, and respond more nimbly to local population health needs without the constraints of annual planning cycles and centralised approval processes.
For patients and communities, the programme should translate into more responsive, locally-tailored services as trusts gain the autonomy to innovate and invest in prevention, community-based care, and digital transformation aligned with the 10 Year Health Plan priorities. The emphasis on population health management and IHO capabilities signals a move toward more integrated, proactive care that addresses health inequalities and keeps people well rather than simply treating illness.
However, success will depend on whether the programme genuinely delivers meaningful freedoms that enable innovation, or becomes another layer of assessment and bureaucracy. The consultation period provides an opportunity to refine the approach, and the phased rollout to 2035 allows for learning and adjustment as the first cohorts progress through the programme.
With the consultation closing on 11 January 2026, this is a critical moment for NHS trusts to engage with and shape the future model of earned autonomy in the health service.
To find the full guide click here.