The Value in Health series from CF explores how the NHS can improve value by delivering better outcomes with the resources available. Drawing on in-depth data analysis, the series aims to understand the relationship between cost, care, and clinical outcomes, and to identify where better resource allocation and service design could, over time, reduce pressure across the system.
There has been growing recognition that addressing unmet need in chronic disease is critical for the sustainability of the NHS. The recently published NHS 10-Year Plan outlines the ambition to deliver more care closer to home, highlighting earlier intervention, prevention, and proactive management of long-term conditions as essential to reducing demand on acute services and delivering better outcomes with the resources available.
However, while the focus is often on reducing acute care pressures, underdiagnosis and suboptimal treatment of long-term conditions represent significant and overlooked drivers of system inefficiency and poor patient outcomes. Reports including the Dash Review have documented widespread care gaps across conditions such as hypertension, diabetes, and respiratory disease. These gaps create a cascade of problems: avoidable deterioration, exacerbations, and emergency admissions that not only place unnecessary strain on acute services but also compromise quality of life.
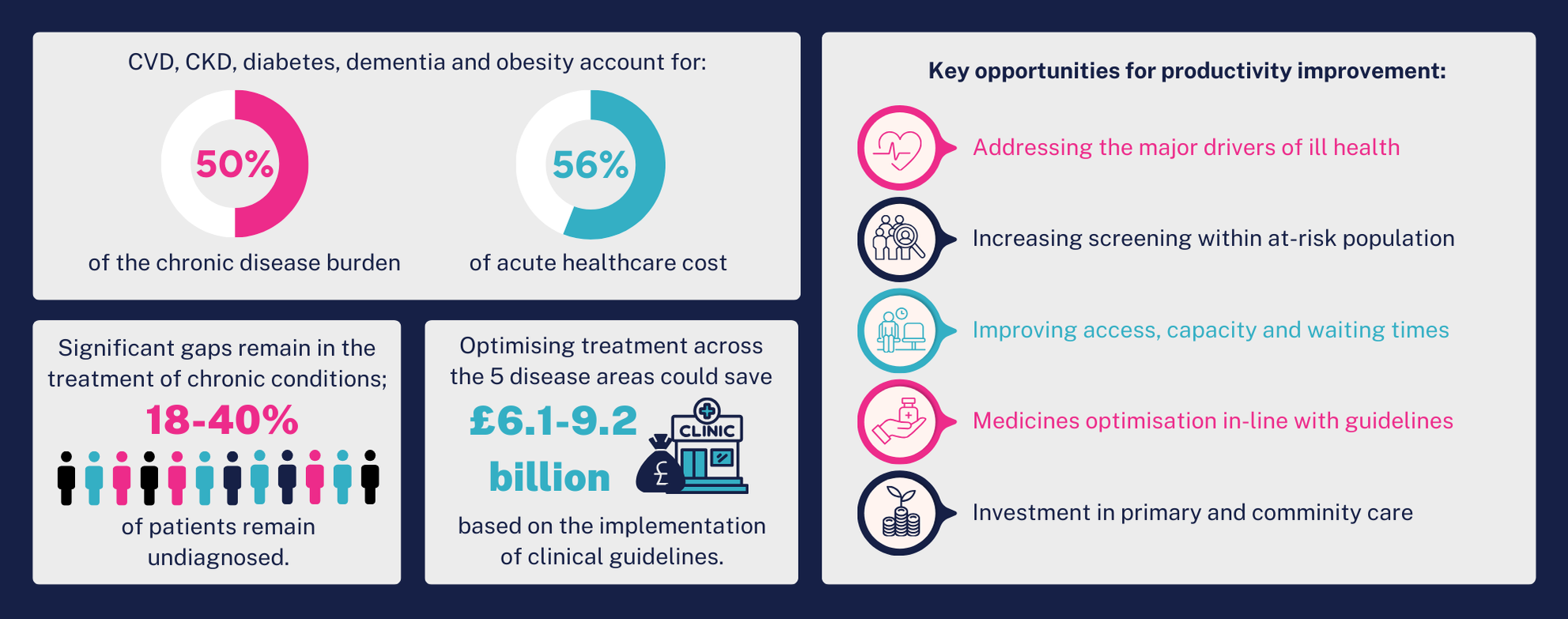
The scale of this opportunity is substantial. Our latest analysis reveals that cardiovascular disease, chronic kidney disease, diabetes, dementia and obesity account for 50% of the chronic disease burden, 26% of acute healthcare costs and 37% of deaths per year, including those with single or multiple conditions. More importantly, there is significant opportunity for improvement: optimising treatment across these five disease areas presents a potential net opportunity of £3.4-£5.0 billion from addressing variation alone, rising to £6.1-£9.2 billion through full implementation of clinical guidelines.
Against this backdrop, this third instalment turns to the opportunity in the treatment of chronic disease, examining the care gaps that arise when long-term conditions are not diagnosed or treated optimally and practical recommendations for how the NHS can begin to capture this value through improved diagnosis, treatment pathways, and care delivery.
What we’ve done – and why
We have focussed on five chronic conditions with significant impact on mortality rates, levels of disability, and healthcare cost: cardiovascular disease (CVD), type 2 diabetes, chronic kidney disease (CKD), obesity, and dementia. Though often analysed independently, these conditions are closely linked, clinically and epidemiologically, with the growing burden of cardio-renal-metabolic (CRM) disease, increasingly associated with the onset of dementia.
These conditions were chosen because of their high prevalence, the severity of health outcomes when left unmanaged, and the existence of proven, cost-effective interventions. They share underlying causes and so commonly co-occur, placing compounded pressure on patients and the healthcare system. Dementia, for example, is now the leading cause of death in the UK, closely followed by CVD (ONS, 2022).
Despite clear clinical guidelines and available treatments, large gaps persist in diagnosis, and in both treatment initiation and optimisation. This results in avoidable mortality and morbidity, and in avoidable costs to the NHS. Our analysis set out to quantify those gaps and explore the potential system savings if care were optimised in line with existing clinical guidance.
A full breakdown of our methodology can be found here.
A closer look
Based on detailed population-level NHS data, our analysis found that the CRM conditions and dementia are significant drivers of mortality, accounting for between 6.5% (obesity) and 37% *(CVD) of deaths each year. Looked at independently, between close to 1 million (dementia) to more than 6 million (obesity) people have a recorded diagnosis within clinical criteria. Independent estimates put the prevalence of these five conditions as significantly higher: beyond those already diagnosed, there is a substantial undiagnosed and at-risk population. If left unaddressed, the burden of disease will continue to grow.
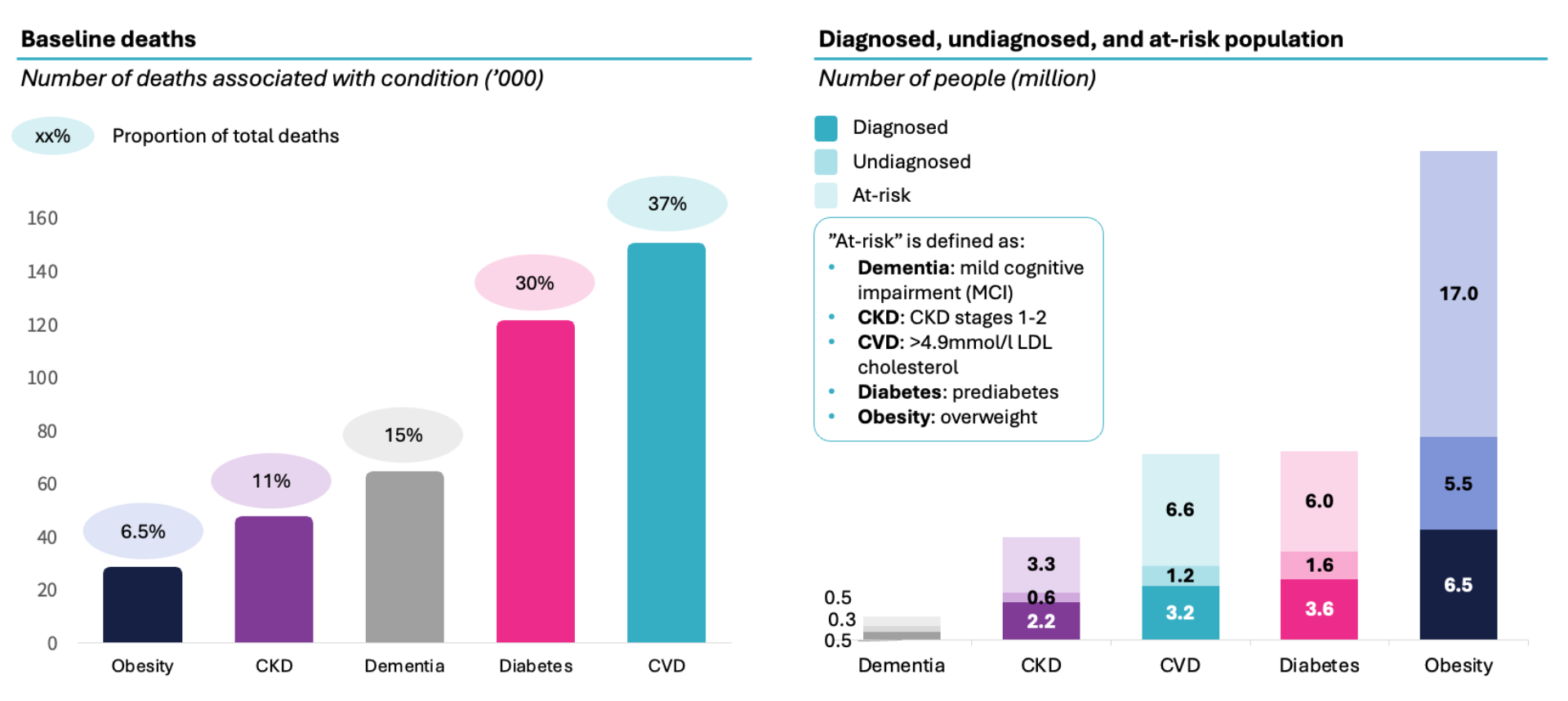
Note: categories overlap in this analysis meaning totals do not add. Source: CF analysis, Diabetes UK, British Heart foundation, Alzheimer’s Society, NHS England, QOF, Gov.uk, ONS, Kidney Research UK, CVD Prevent.
In addition to heart attacks, strokes and deaths, largely preventable chronic disease places an increasing strain the health system, especially the acute sector, with increased A&E attendances, emergency admissions and outpatient appointments. It has been complicated to understand the precise burden of these conditions together due to the substantial comorbidity of disease—and previous attempts to do so have used subsets of the population or estimates.
In new analysis of record-level data of the whole population, we find that individuals with a single long-term condition make up 6.8% of the population and account for 7.9% of NHS acute costs, while those with multimorbidity represent 15% of the population but drive 39.7% of acute costs; together 22% of the population drive 48% of costs. Meanwhile, while dementia affects just over 1% of the population yet accounts for 10% of acute spend.
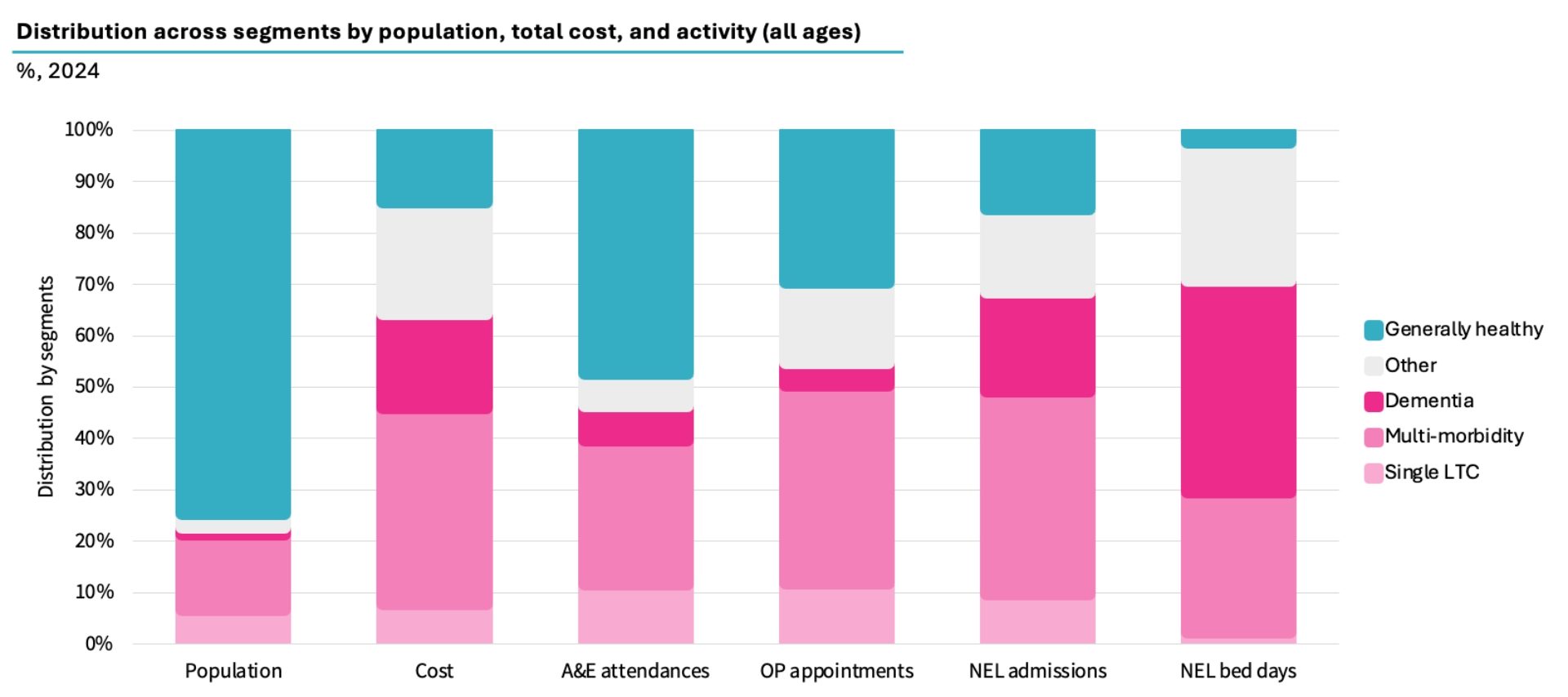
Further analysis focussed on the four major chronic conditions—cardiovascular disease, diabetes, chronic kidney disease, and obesity—and on dementia. These CRM conditions account for £26 billion or 50% of the chronic disease burden and 56% of acute healthcare cost, with dementia contributing an additional £8 billion, for a total of £34bn.
Source: CF Population Segmentation using analysis of ONS, Hospital Episode Statistics record level data, National Cost Collection Index, MFF.
In theory, the NHS is well positioned to manage these conditions: NICE has developed world-leading guidance on cost-effective care in all five areas. But in practice, there are large and measurable gaps between expected prevalence and what is diagnosed, treated, and optimised. These gaps that must be closed to better meet the needs of the population.
Our analysis revealed that only 37% of people with cardiovascular disease have cholesterol below target and only 28% of people with diabetes are at the optimal level of blood sugar control. Less than 20% of CKD patients receive medication, and stage 1 and 2 CKD are not addressed by NICE guidance representing a lost opportunity to intervene and modify disease progression. In obesity and dementia, most of the eligible population do not even receive treatment. 65% of dementia patients are diagnosed and only 5% of patients are on AcHe inhibitors which has been shown to delay admission to residential care by up to 2 years. Moreover, recent evidence suggests that 45% of risk factors of dementia are addressable and hence dementia could be prevented largely by addressing the same CVRM risk factors.
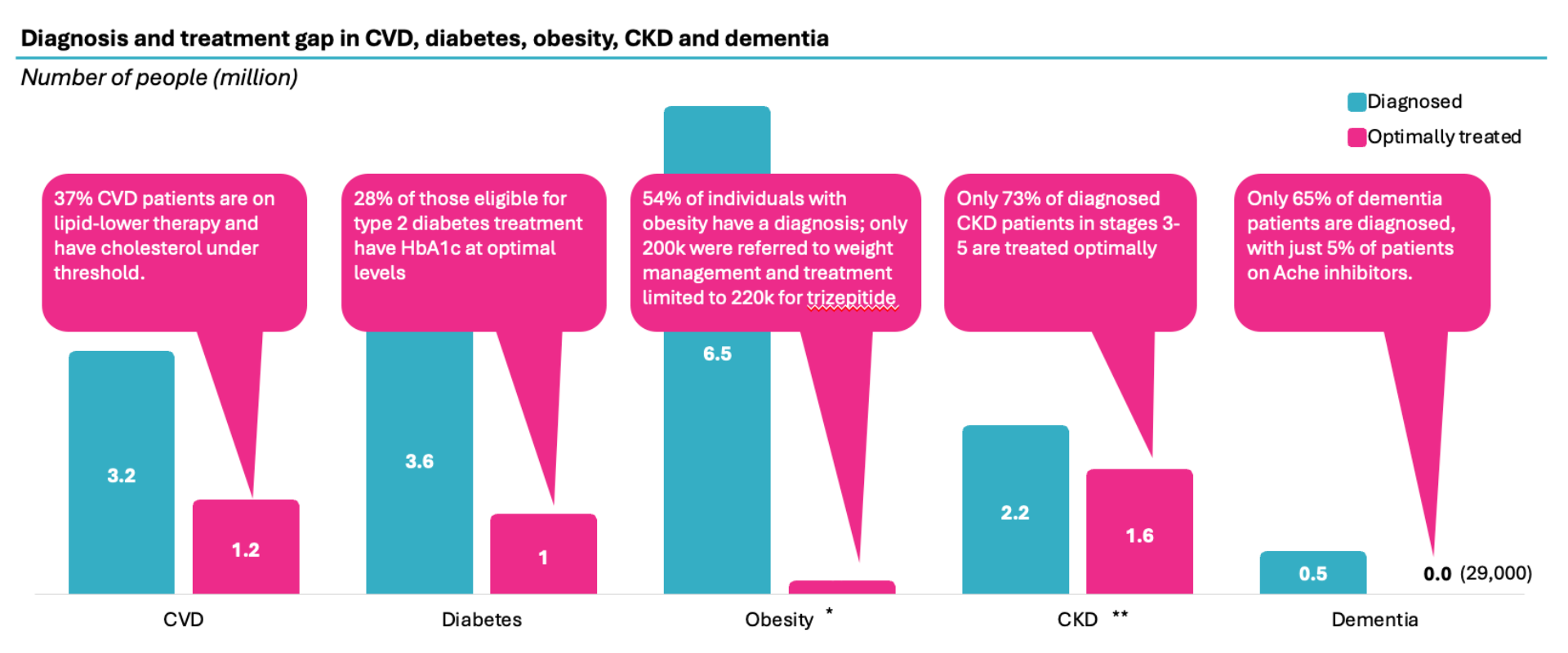
*Treatment statistics for obesity were not included as targets for obesity are subjective and differ for each individual. **Treatment statistics for CKD were not included as the number of people on CKD medicines (independent of dialysis and/or transplant) are not widely reported. Sources: CVD: CVDPREVENT, Health Survey England; NHSBSA; British Heart Foundation; Diabetes: QOF, NHSE, ONS; Obesity: Gov.UK, QOF, National Obesity Audit; CKD: Kidney Research UK, QOF; Dementia: NHSE Primary Care Dementia Data, DiscoverNOW, QOF, CF analysis
If more patients with high cholesterol achieved recommended LDL levels through appropriate treatment, the NHS could avoid an estimated 6,500 deaths and save up to £4.8 billion annually. Improved glycaemic control in people with diabetes could prevent up to 10,000 strokes and heart attacks, 1,600 amputations, and yield £1.6 billion in savings. In obesity, a modest reduction in prevalence would not only prevent thousands of cardiovascular deaths but also generate savings of £1.5 billion. Slowing the progression of dementia could defer the need for care home admission by two years, saving an estimated £1.8 billion. For CKD, earlier and broader medication use could reduce cardiovascular complications and associated hospitalisations, although precise cost savings were more difficult to quantify due to current data limitations.
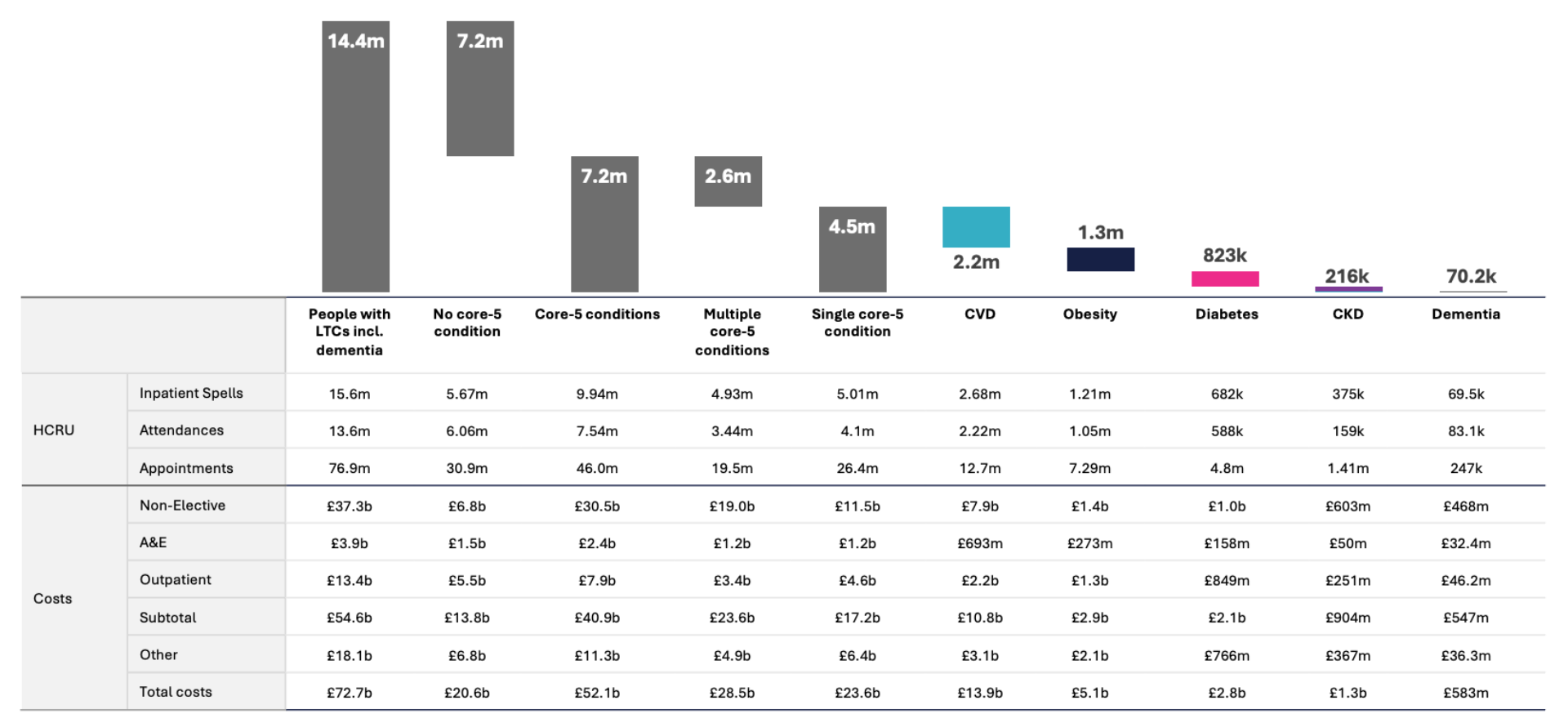
To accurately quantify the total opportunity, it is important to account for the high level of comorbidity across these conditions. Therefore, we have analysed segments of the population; people with single long-term conditions, those with multimorbidity, and those living with dementia.
Our analysis shows that optimising treatment has the potential to reduce HCRU costs and mortality across the five health conditions with potential gross savings between £870 million to £4.8 billion, and that is before considering any longer-term impact from heart attacks, strokes etc. This used two different methods: 1) variation analysis within similar conditions, controlling for age and deprivation, and 2) risk reduction based on the achievement of clinical guidelines and reducing underlying drivers of disease.
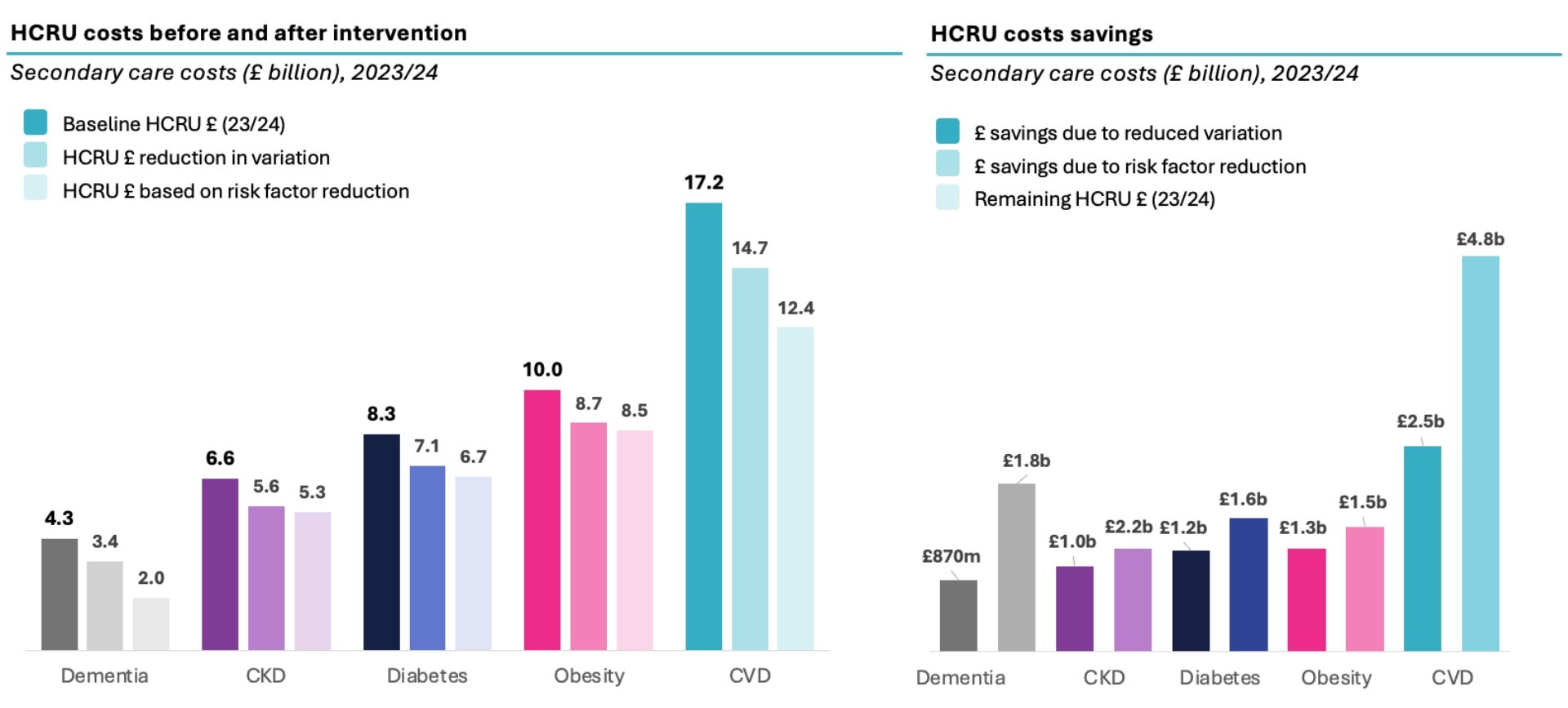
Source: HES APC, ECDS, OP; CF analysis; CVD: NHSE, ONS, CVDPREVENT, Health Survey England; Diabetes: BNF, NHSE, QOF, ONS, diabetes.co.uk; CKD: Kidney Research UK, CVDPREVENT, Ku et al. (2018); Obesity: GOV.UK, QOF, Jensen et al. (2024); Dementia: QOF, Zuin et al. (2022), Xu et al. (2021), Davis et al. (2018)
While these opportunities cannot simply be added, applying the average gross opportunity rate of 15% (for the variation method) to 29% (based on risk reduction) to the total £34b spend on CVRM and Dementia would be worth £4.7-9.0b. Extending the rate of CVRM savings to non-CVRM chronic conditions would take the total to £6.7 to £12.3b in total. Reinvesting 25-50% of the savings in identifying and managing patients appropriately would still produce a net opportunity of £3.4b-£5.0b from pure variation and £6.1-£9.2b based on the implementation of clinical guidelines.
What needs to change?
We have identified five areas where intervention would drive the realisation of some of this opportuntity:
Implications beyond acute care
While our analysis focused on acute healthcare costs within the NHS, it is likely that broader benefits across the health and care system would be even greater. Better management of chronic disease would reduce pressure on primary and community care, lower the burden on social services, and improve workforce participation by reducing long-term sickness and early retirement. Crucially, it would also improve quality of life for millions—preserving mobility, independence, and wellbeing in older age.
A model for prevention and population health
Emerging models of protocolised care offer a roadmap. In parts of the country, CVD management is already being delivered by pharmacists co-located with vaccination centres—streamlining care and improving access. These initiatives offer a template for extending CRM and dementia management into primary care settings and local hubs.
For CVD in particular, a more consistent and data-driven “ABC” model (Atrial fibrillation, Blood pressure, Cholesterol) can improve both outcomes and resource use. By shifting elements of care to trained non-medical professionals, supported by digital tools and administrative teams, ICBs can achieve more with limited clinical time—while building the governance required for population-scale delivery.
Looking ahead
This report captures only a fraction of the full opportunity. It focuses on acute care savings and excludes primary, community, and social care benefits. It measures one-year impacts, but the benefits of optimised chronic disease management will compound over time—reducing admissions, improving quality of life, and supporting economic productivity through a healthier workforce.
Ultimately, closing the care gaps in CRM and dementia is both clinically essential and economically sound. The NHS cannot afford to leave these needs unmet. With targeted investment, structured delivery models, and the full use of available data and treatments, there is a clear path to delivering better health—and better value—for the population.
About CF
CF is a leading consultancy dedicated to making an enduring impact on health and healthcare. We work with leaders and frontline teams to improve health, transform healthcare, embed life science innovation and boost growth through investment. With unmatched access to UK healthcare data and award-winning data science expertise, our team are a driving force for delivering positive and meaningful change.
About the authors

Ben Richardson
Ben Richardson is a Managing Partner at CF, leading Life Sciences and Data Innovation. With two decades of experience, he has worked with health systems and life sciences companies globally, focusing on strategy, transformation, and development. Ben has contributed to primary care, diabetes, cardiovascular, cancer, mental health, and population health management. Since 2014, he has helped CF become an award-winning healthcare company in management consulting and data services.

Jo Andrews
Jo is the Chief Medical Officer at CF. His decade at CF, working across health systems and the life sciences sector builds on a 23 year career as a practicing clinician in the NHS. He works extensively with clinicians and multidisciplinary teams, using data to identify opportunities to improve care and outcomes through the design and delivery of patient -centred care pathways.

Yemi Oviosu
Yemi is a Senior Manager at CF with a PhD in Cardiovascular Biochemistry, specialising in strategy and scaling innovation for healthcare and life sciences clients. He focuses on evaluating and implementing digital technologies that enable population health management and driving sustainable, enterprise-wide transformation. His unique blend of scientific insight and technology-strategy expertise helps clients accelerate innovation, de-risk investments, and improve patient outcomes.
With special thanks to Elise Kearsey, Beena Mistry, Dike Adaluso, Sarah Sharer, Colette Russell, Lali Sindi and Gauri Patel.






