The NHS in England planned to spend around £14.8bn providing Mental Health services in 2021/22, with £2.3bn coming from NHS England specialised commissioning and £12.5bn from local CCG budgets. This represented 14.8% of the total funds allocated to CCGs for health services. Around 1.5 million people are in contact with Mental Health services each month. Improving Mental Health is a clear priority for the government and our health and care systems. The Covid-19 pandemic has also heightened recognition of the importance of Mental Health. However, services are facing significant challenges from increasing demand, the need to tackle inequalities, a lack of integration with other health and care provision, as well as persistent funding inequity.
Mental Health services are experiencing significant increase in demand
The number of referrals to Mental Health services each year is rising at a rate that outstrips population growth. We know that demand for Mental Health support has been exacerbated by the Covid-19 pandemic and that 2021 saw a record 4.3 million referrals to specialist Mental Health services.
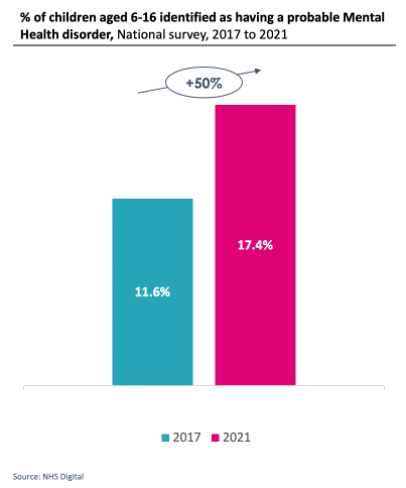
Child and Adolescent Mental Health services (CAMHS) are among those seeing the highest rates of growth in demand. Nationally, the Covid-19 pandemic has been linked with a deterioration in children’s mental health and wellbeing, which is likely to have a continued impact on increasing demand for services over the next few years. A national survey across England in 2021 identified that 17% of children and young people aged between 6-16 had a probable Mental Health disorder. This was a 50% increase from the 12% of children and young people identified as having a probable mental health disorder in an equivalent survey carried out in 2017.
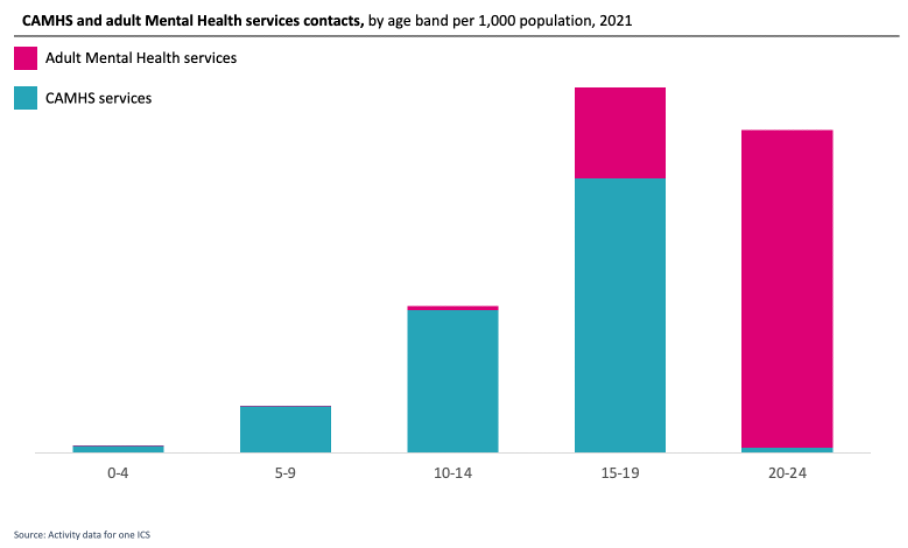
While children’s and young people’s mental health services are in the spotlight, there is an opportunity to ensure that pathways are providing proactive and preventative support at an early age, as well as to help young people as they turn 18. There is a national priority to improve the transition process from CAMHS to adult Mental Health services. What we can see at the moment is a drop off in the number of Mental Health service contacts for young people between the ages of 15-19 and 20-24. This may be because some young people are slipping through gaps during the transition period. If young people are unable to access the support they need at this crucial time, this will increase the likelihood of their condition deteriorating and escalating into crisis.
There are also clear inequalities in service provision, access and activity across the country
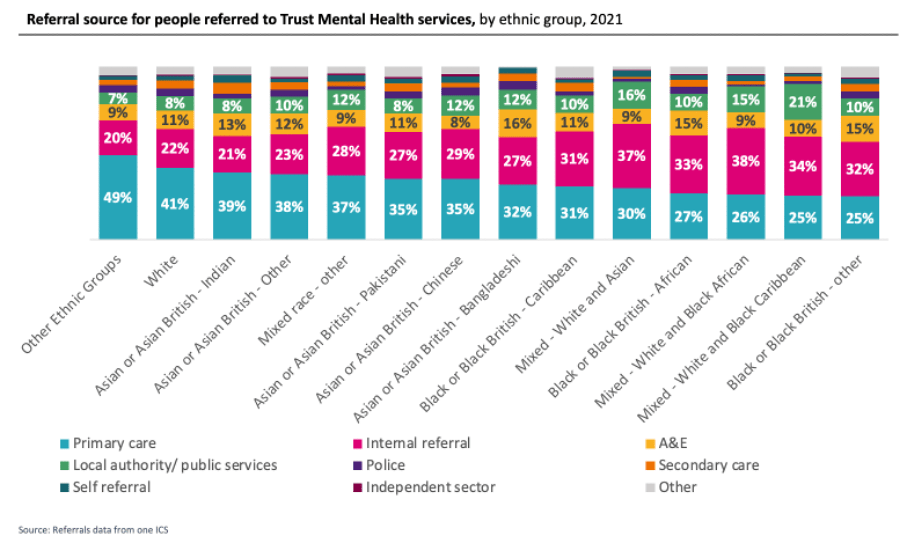
Where you live affects the services you have access to, how long you wait for treatment and the outcomes you can expect. We also know that this appears to impact people from ethnic minorities differently. Services are not meeting the needs of some of the cultures within the community and therefore some communities disproportionately experience crisis or are not able to access services. For example, people from ethnic minorities are more likely to present in A&E and arrive in Mental Health inpatient wards with higher acuity or be detained under the Mental Health Act.
A higher proportion of people from white ethnic groups are referred to secondary Mental Health services from primary care, while people from ethnic minorities are more likely to access secondary services after attending A&E.
Black population groups have more contacts with secondary Mental Health teams, and they are more likely to be admitted than seen by crisis teams.
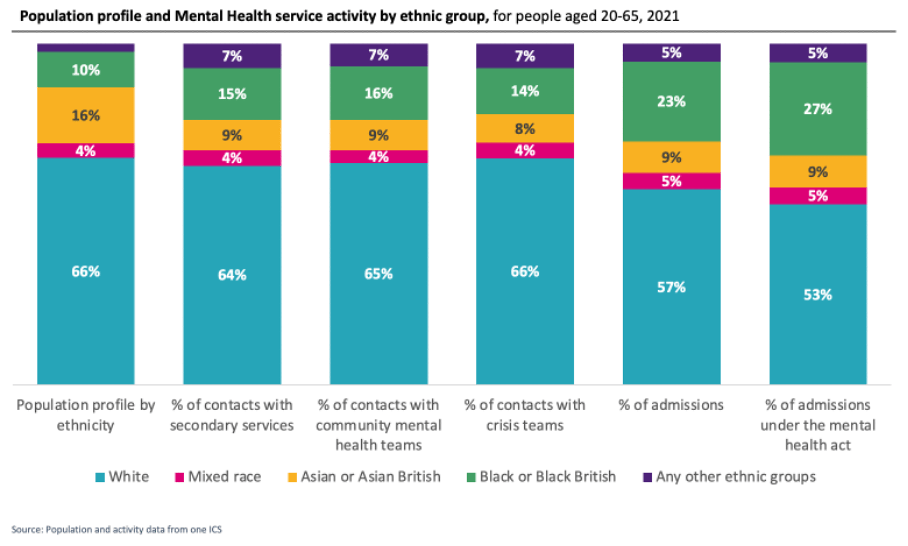
There is a need to understand the cultural sensitivity of services offered and why certain groups are less likely to access support, particularly the Asian/Asian British community.
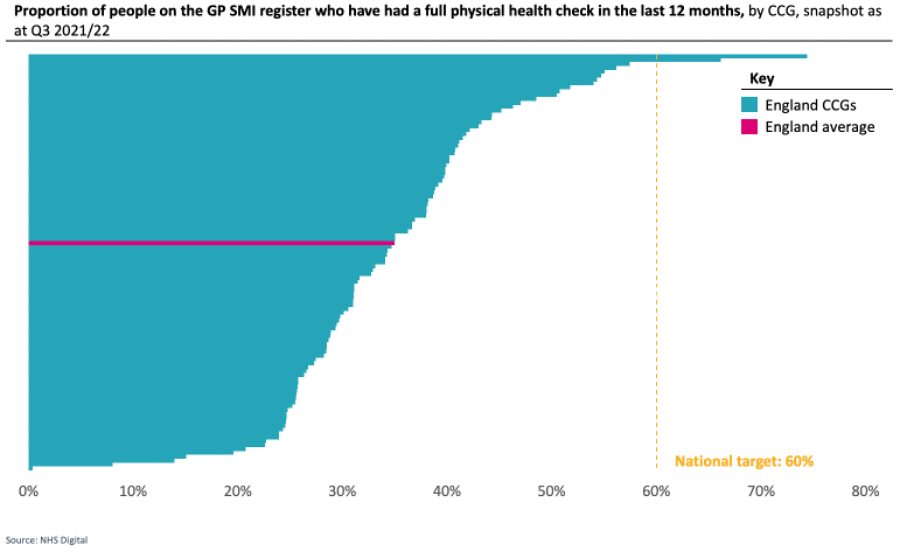
More work is needed to care jointly for Mental Health and Physical Health
The ambition of many health systems is to provide holistic care, that enables people’s different health and care needs to be met in a joined-up way. We know that Physical Health and Mental Health are often closely interlinked, and people often experience co-morbid Physical Health and Mental Health conditions. Research has shown that people with Severe Mental Illness die on average 15-20 years earlier than the general population. However, across England at the end of Q3 2021/22, only 35% of people with SMI had received all their physical health checks in the last 12 months. This compares to a national target of 60%. As at Q3 2021/22, this target was only met by 2 CCGs in England.
If someone is admitted to an acute hospital for an urgent physical health need, but who also has a mental health diagnosis, they tend to spend longer in hospital before they are discharged. This is particularly apparent for children and young people (under 18s) and older people (over 65s), who on average spend over 25% longer in hospital. For older people, this may link with dementia diagnosis and the challenge of arranging appropriate longer-term care in the community.
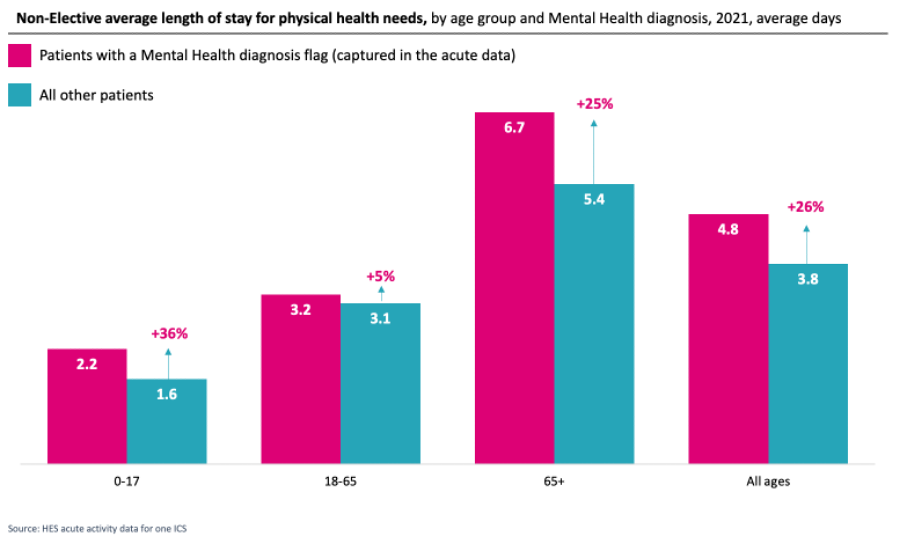
There is an opportunity to improve holistic care for people so that their Mental Health and Physical Health needs are being cared for jointly.
Despite funding increases for Mental Health services, inequities remain
Investment in Mental Health services has increased significantly in recent years. All CCGs are now expected to meet the Mental Health Investment Standard at a minimum, meaning that investment in Mental Health services must increase in real terms in line with the overall funding allocation. Recent publications of strategy and policy by the government and NHS organisations have also committed increased funding.
However, given the increasing demand, which has been particularly significant as a consequence of the pandemic, funding must stretch even further. This challenges systems about how they can invest in service improvements and transformation. For example, being able to invest upfront into more proactive and preventative care would lead to improvements in outcomes for residents and financial savings, but over a longer-term timeframe.
In addition, there is clear funding inequity between CCGs in England. When taking the relative level of need of the population into account, spend per head on Mental Health services ranges from just over £300 to just under £150.
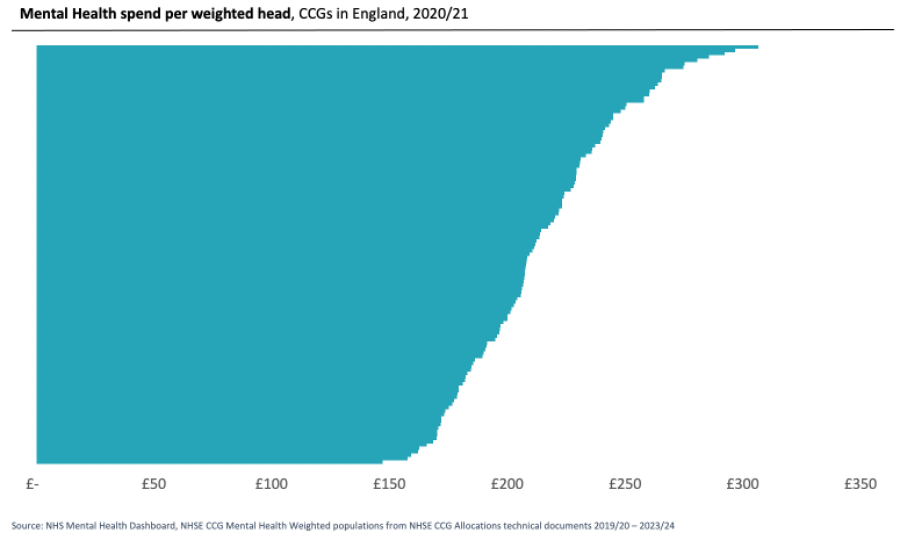
Newly formed ICS’s, often with recently merged CCGs, will encounter historic commissioning arrangements and levels of funding for their populations overall, that are not addressed through the MHIS, given the restrictions in how it is applied. This perpetuates variation in the level of funding proportionate to the level of need of the population – and that applies to different ICS’s and also between different geographies within the same system. This has a knock-on impact on the services residents are able to access and the outcomes they can expect, which is not tenable. Against a background of financial pressure, there is a challenge for how systems can resolve this inequity.
As the new ICS’s form, there is an opportunity for Mental Health, Community Health and Secondary Care providers, Primary Care and Local Authorities to align their Mental Health strategies, and work together to tackle the challenges facing services. Provider Collaboratives may be able to support the delivery of services targeted to meet the needs of local populations, and strategically direct investment to support those who need it most.




