Creating shared accountability in ICSs for improved outcomes
Integrated Care Systems (ICSs) have been set up to facilitate collaboration across health, care and local organisations within a system to improve population health outcomes, reduce health inequalities, enhance productivity and support social and economic development. There is a commitment from NHS England to embed “system by default” as the way for managing. To do so, the new arrangements need to find a way to embrace the exciting potential for ICSs to serve as a vehicle for collaboration between local government, the NHS and a range of other actors, as well as for decision-making around the use of collective resource. In turn, this requires creating accountability for use of public resources and raises questions about how we can most effectively use data to improve performance.
With ICSs now live, they are evolving ways to manage system oversight and progress against their four core purposes outlined above.[i] This oversight needs to embody the collaborative nature of ICSs, moving towards a more system-wide mindset with shared responsibility for performance and a risk proportionate approach. Permissive system oversight is needed that embeds collective accountability and shared outcomes, and brings the system together to tackle challenges such as inequalities. In a survey of ICS leaders by the NHS Confederation (published 10 February 2022) 20% of respondents selected oversight and regulation as one of the biggest obstacles to ICS progress over the coming years.[ii]
Building a system-wide approach to improving performance against outcomes
The Integrated Care Board (ICB) needs to create the right incentives for system-owned performance and continuous improvement, in a framework where they can both discharge their duties and act as a foundation for driving collaboration. A balance needs to be struck between empowering providers to manage, oversee and address their own and others’ performance, and providing the necessary confidence and oversight at different levels (with options for intervention when required). This balance applies to all aspects of oversight, from governance and responsibilities to assurance and reporting lines; whether for resource allocation, monitoring service quality and access, or reviewing wider system integration and health outcomes.
Reflecting the vision set out in the ICS Design Framework[iii], system improvement relies on collective accountability across health and care providers, moving away from an organisational mindset. There is a real opportunity for stronger peer support and challenge amongst providers, in part by sharing best practice, aligning around shared outcomes and holding one another to account in delivering these. ICSs also need to address the wider barriers to accountability. For example, we know the critical role the VCSE sector plays in filling gaps in services that meet essential local needs, but short-term funding for these services can limit their accountability in the system.
Finally, the oversight framework should foster a clear understanding of the role that every individual organisation at a place-based level plays in overall system performance. This should be reflected in both the governance and metrics, bringing health and care partners together to address health inequalities and taking a more holistic approach that draws on the sectors outside of health that we know shape outcomes. ICSs will need to consider opportunities beyond existing frameworks such as the System Oversight Framework (SOF) which only applies to NHS organisations. In turn, this supports broader social and economic development, combined with the ICS’s role as a key anchor institution.
Learning from different models and sectors
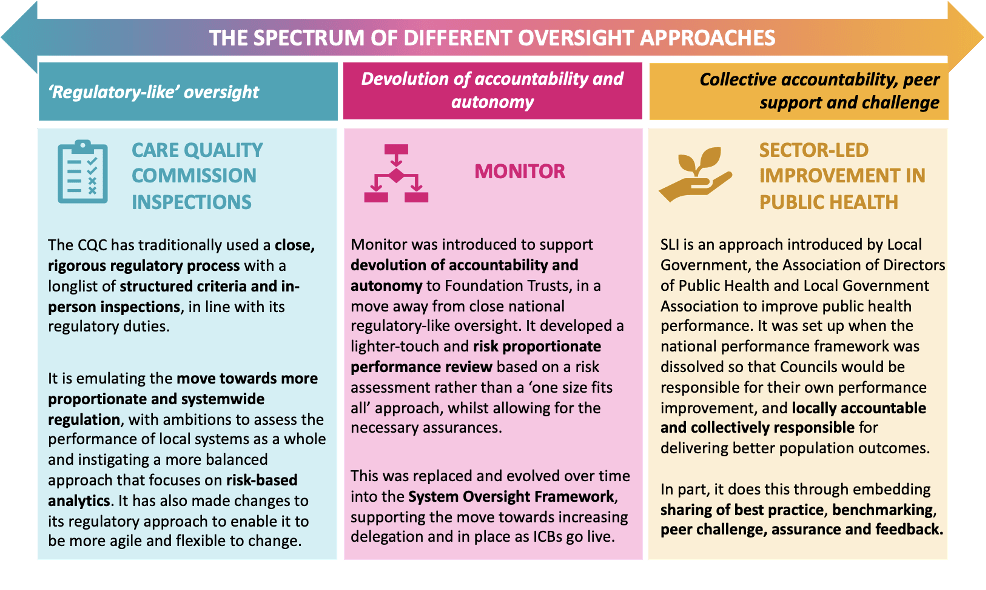
There are many examples of different oversight frameworks – both in the UK and globally – that sit along a spectrum of more top-down, directive system management, through to lighter-touch more devolved responsibility, and collective responsibility and challenge. Take the different approaches seen across Monitor (now evolved into the SOF) and CQC in the NHS, and Sector-Led Improvement in public health, illustrated in Figure 1.
The direction of travel in provider oversight has been increasing delegation and local accountability, with increasing responsibility being passed to ICBs from the centre, and in turn from ICBs to provider collaboratives and places. This move towards more proportionate and systemwide oversight is being emulated at all levels of health and care.
Setting the right priorities for your ICS
System oversight is not just about governance, and rests upon the ability to focus on the right areas that support change. Our Insights & Collaboration Engine demonstrates how routinely accessed, ICS-wide datasets can be used to monitor broader progress and integration against shared metrics. It enables ICSs to understand barriers to service integration and better shared population outcomes within their own geographies, and to compare themselves to their peers by collating metrics across three chasms: physical and mental health, acute and community care, and health and social care.
So which framework is the right choice?
From our discussions across ICSs and providers in the NHS, Local Government and beyond, many are aiming to position themselves on the righthand side of the spectrum but in some cases find themselves coming up against the left of regulatory, targets-driven oversight. In this case, it is essential that in designing their approach, ICSs consider:
- Their system context – current providers and performance, service infrastructure and population needs
- Availability of real-time data (and furthermore, shared data) and how this is used to drive shared learning and change
- The existing burden on the system, particularly following the operational pressures and high demand created by the Covid-19 pandemic
- Capability and capacity – systemwide performance improvement and progress against population health outcomes requires the right skills and leadership, including the skillsets to assimilate and use data for oversight and decision-making
- Clear and transparent governance – clarity on how information flows and accountability works at every level within the system
Getting the system oversight, shared outcomes and collective accountability right should lead to improved productivity, drawing on what all of the organisations within an ICS can offer as a sum of its parts, and aligning and empowering them around shared goals that improve population health.
[i] NHSEI; Integrating Care: Next steps to building strong and effective integrated care systems across England; November 2022
[ii] NHS Confederation; The state of integrated care systems 2021/22; February 2022
[iii] NHSEI; Integrated Care Systems: Design Framework; June 2021


